Introduction
The NHSScotland National Infection Prevention and Control Manual (NIPCM) was first published on 13 January 2012, by the Chief Nursing Officer (CNO (2012)1), and updated on 17 May 2012 (CNO (2012)1 Update).
The NIPCM provides IPC guidance to all those involved in care provision and is considered best practice across all health and care settings in Scotland.
The re-launch of the NIPCM by the CNO on 11 July 2022 emphasises the ongoing importance of application of Infection Prevention and Control (IPC) guidance within health and care settings across Scotland.
Video of Chief Nursing Officer re-launching the NIPCM
Find out more about the NIPCM
You can find out more about the NIPCM by watching the animation or going to the About the manual webpage.
Disclaimer
When an organisation, for example health and care setting, uses products or adopts practices that differ from those stated in this National Infection Prevention and Control Manual, that individual organisation is responsible for ensuring safe systems of work including the completion of a risk assessment approved through local governance procedures.
Responsibilities
Responsibilities for the content of this manual
ARHAI Scotland must ensure
- that the content of this manual remains evidence based or where evidence is lacking, content is based on consensus of expert opinion.
Stakeholders of the ARHAI Scotland programmes must ensure
- full participation in the working groups and oversight programmes including full engagement with the consultation process outlined in the Terms of Reference associated with each group
Responsibilities for the adoption and implementation of this manual
Organisations must ensure:
- the adoption and implementation of this manual in accordance with their existing local governance processes
- systems and resources are in place to facilitate implementation and compliance monitoring of infection prevention and control as specified in this manual in all care areas
- compliance monitoring includes all staff (permanent, agency and where required external contractors)
- there is an organisational culture which promotes incident reporting and focuses on improving systemic failures that encourage safe infection prevention and control working practices including near misses
Managers of all services must ensure that staff:
- are aware of and have access to this manual
- have had instruction/education on infection prevention and control through attendance at events and/or completion of training (for example via NHS Education for Scotland (NES) and/or local board or organisation)
- have adequate support and resources available to enable them to implement, monitor and take corrective action to ensure compliance with this manual. If this cannot be implemented a robust risk assessment detailing deviations from the manual and appropriate mitigation measures must be undertaken and approved through local governance procedures.
- with health concerns (including pregnancy) or who have had an occupational exposure relating to the prevention and control of infection are timeously referred to the relevant agency, for example General Practitioner, Occupational Health or if required Accident and Emergency
- have undergone the required health checks or clearance (including those undertaking Exposure Prone Procedures (EPPs)
- include infection prevention and control as an objective in their Personal Development Plans (or equivalent)
Staff providing care must ensure that they:
- understand and apply the principles of infection prevention and control set out in this manual
- maintain competence, skills and knowledge in infection prevention and control through attendance at education events and/or completion of training, for example NHS Education for Scotland (NES) and/or local board or organisation
- communicate the infection prevention and control practices to be taken to appropriate colleagues, those being cared for, relatives and visitors without breaching confidentiality
- have up to date occupational immunisations/health checks/clearance requirements as appropriate
- report to line managers and document any deficits in knowledge, resources, equipment and facilities or incidents that may result in transmission of infection including near misses e.g sharps or PPE failures
- do not provide care while at risk of potentially transmitting infectious agents to others - if in any doubt they must consult with their line manager, Occupational Health Department, Infection Prevention and Control Team (IPCT) or Health Protection Team (HPT)
- contact HPT/IPCT if there is a suspected or actual HAI incident/outbreak
Infection Prevention and Control Teams (IPCTs) and Health Protection Teams (HPTs) must:
- engage with staff to develop systems and processes that lead to sustainable and reliable improvements in relation to the application of infection prevention and control practices
- provide expert advice on the application of infection prevention and control in all care settings and provide support to develop individual or organisational risk assessments where deviations from the NIPCM are necessary
- have epidemiological or surveillance systems capable of distinguishing patient case or cases requiring investigations and control
- complete documentation when an incident/outbreak or data exceedence is reported (IPCTs should ensure application of the HIIAT where applicable and report incidents and outbreaks using the ORT as outlined by the HIIAT).
Last updated: 4 October 2021
Chapter 1 - Standard Infection Control Precautions (SICPs)
 Standard Infection Control Precautions (SICPs), covered in this chapter are to be used by all staff, in all care settings, at all times, for all patients1 whether infection is known to be present or not to ensure the safety of those being cared for, staff and visitors in the care environment.
Standard Infection Control Precautions (SICPs), covered in this chapter are to be used by all staff, in all care settings, at all times, for all patients1 whether infection is known to be present or not to ensure the safety of those being cared for, staff and visitors in the care environment.
The Hierarchy of Controls should also be considered in controlling exposures to occupational hazards which include infection risks.
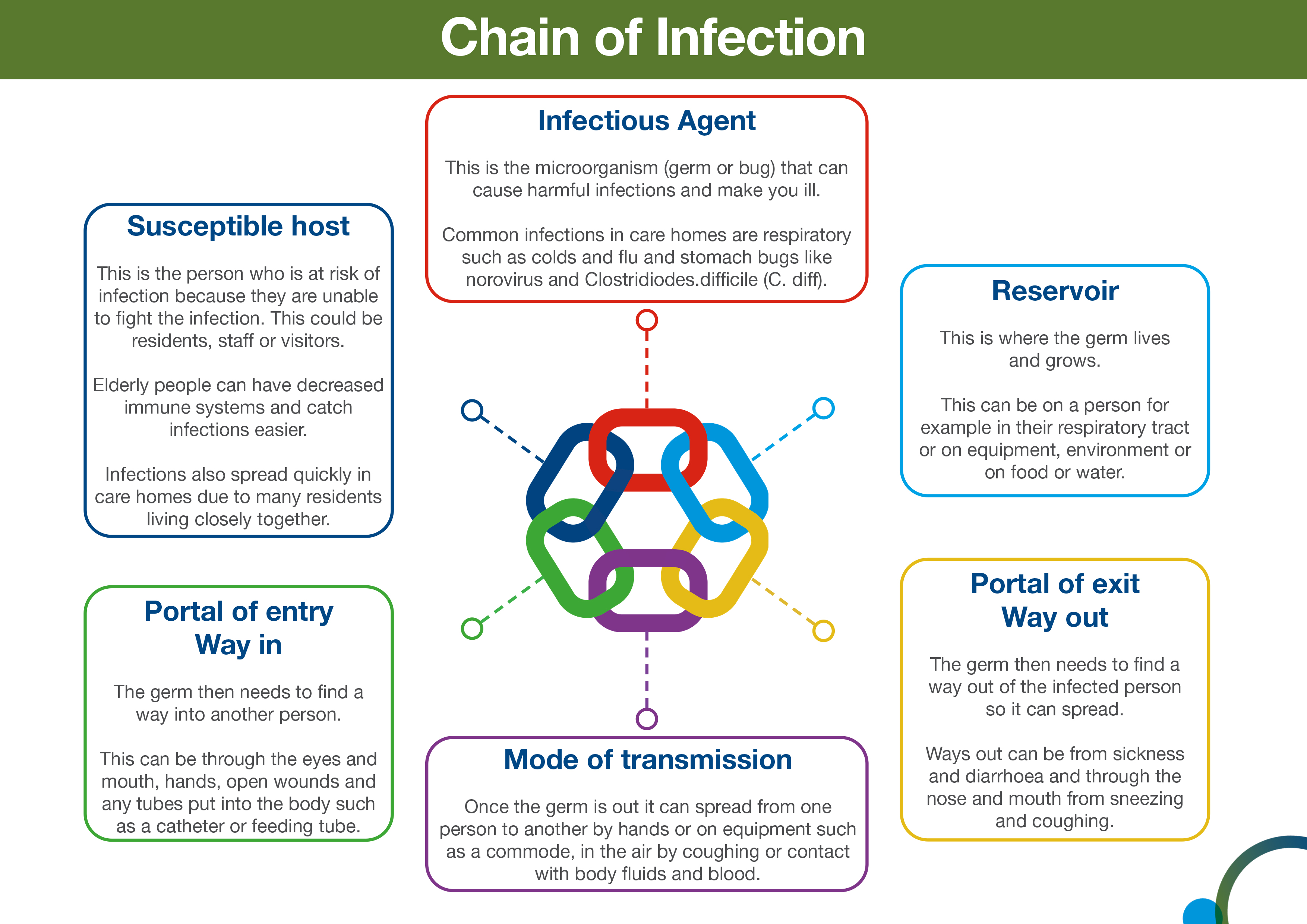
SICPs are the basic infection prevention and control measures necessary to reduce the risk of transmission of infectious agent from both recognised and unrecognised sources of infection.
Sources of (potential) infection include blood and other body fluids secretions or excretions (excluding sweat), non-intact skin or mucous membranes, any equipment or items in the care environment that could have become contaminated and even the environment itself if not cleaned and maintained appropriately.
The application of SICPs during care delivery is determined by an assessment of risk to and from individuals and includes the task, level of interaction and/or the anticipated level of exposure to blood and/or other body fluids.
To be effective in protecting against infection risks, SICPs must be applied continuously by all staff. The application of SICPs during care delivery must take account of;
- risk to and from the individual for whom care is being provided
- the task to be undertaken
- level of interaction
- the anticipated level of exposure to blood and/or other body
Doing so allows staff to safely apply each of the 10 SICPs by ensuring effective infection prevention and control is maintained.
SICPs implementation monitoring must also be ongoing to demonstrate safe practices and commitment to patient, staff and visitor safety.
Further information on using SICPs for Care at Home can be found on the NHS National Education Scotland (NES) website.
1The use of the word 'Persons' can be used instead of 'Patient' when using this document in non-healthcare settings.
Last updated: 28 August 2023
1.1 Patient Placement/Assessment for infection risk
Patients must be promptly assessed for infection risk on arrival at the care area (if possible, prior to accepting a patient from another care area) and should be continuously reviewed throughout their stay. This assessment should influence patient placement decisions in accordance with clinical/care need(s).
Patients who may present a particular cross-infection risk should be isolated on arrival and appropriate clinical samples and screening undertaken as per national protocols to establish the causative pathogen. This includes but is not limited to patients:
- With symptoms such as loose stools or diarrhoea, vomiting, fever or respiratory symptoms.
- With a known (laboratory confirmed) or suspected infectious pathogen for which appropriate duration of precautions as outlined in A-Z pathogens are not yet complete.
- Known or suspected to have been previously positive with a
Multi-drug Resistant Organism (MDRO), for example MRSA, CPE. - Who have been a close contact of a person who has been colonised or infected with CPE in the last 12 months.
- Who have been hospitalised outside Scotland in the last 12 months (including those who received dialysis).
Resources
For assessment of infection risk see Section 2: Transmission Based Precautions.
Further information can be found in the patient placement literature review.
Further information regarding general respiratory screening questions can be found within the resources section of the NIPCM.
1.2 Hand Hygiene

Please note that the term ‘alcohol-based hand rub (ABHR)’ has now been updated to ‘hand rub’. A hand rub (alcohol or non-alcohol based) can be used if it meets the required standards. Please see further information in the hand hygiene products literature review.
Hand hygiene is considered an important practice in reducing the transmission of infectious agents which cause infections.
Hand washing sinks must only be used for hand hygiene and must not be used for the disposal of other liquids. (See Appendix 3 of Pseudomonas Guidance)
Before performing hand hygiene:
- expose forearms (bare below the elbows)
- remove all hand/wrist jewellery* including any embedded jewellery (a single, plain metal finger ring or ring dosimeter (radiation ring) is permitted but should be removed (or manipulated) during hand hygiene). Bracelets or bangles such as the Kara which are worn for religious reasons should be able to be pushed higher up the arm and secured in place to enable effective hand hygiene which includes the wrists
- ensure fingernails are clean, short and that artificial nails or nail products are not worn
- cover all cuts or abrasions with a waterproof dressing
Hand washing should be extended to the forearms if there has been exposure of forearms to blood and/or body fluids.
*For health and safety reasons, Scottish Ambulance Service Special Operations Response Teams (SORT) in high-risk situations require to wear a wristwatch.
To perform hand hygiene
Hand rubs must be available for staff as near to point of care as possible. Where this is not practical, personal hand rub dispensers should be used.
Application of sufficient volume of hand rub to cover all surfaces of the hands is important to ensure effective hand hygiene. Manufacturer’s instruction should be followed for the volume of hand rub required to provide adequate coverage for the hands. In the absence of manufacturers instructions, volumes of approximately 3ml are recommended to ensure full coverage.
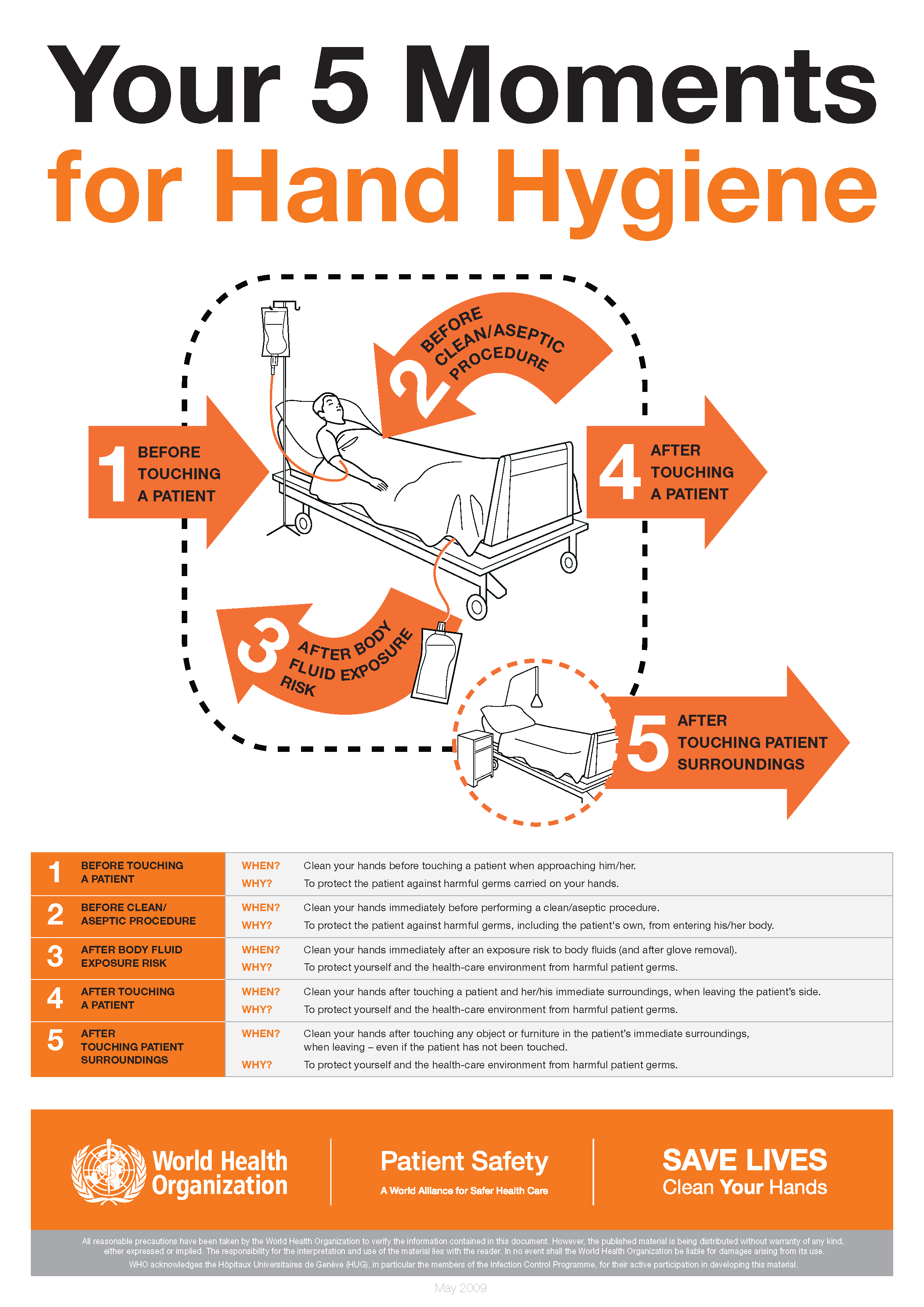
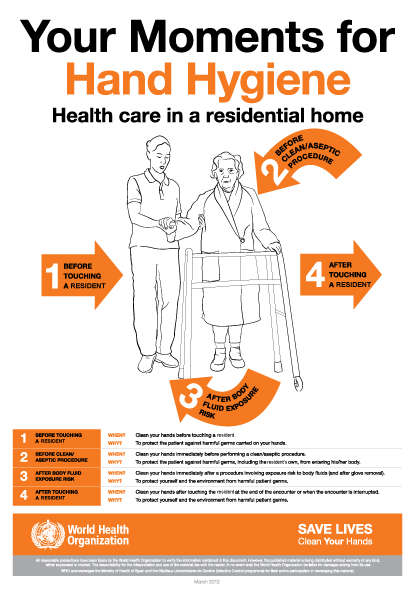
The World Health Organization’s ‘5 moments for hand hygiene’ should be used to highlight the key indications for hand hygiene.
- before touching a patient
- before clean/aseptic procedures. If hand rub cannot be used, then antimicrobial liquid soap should be used
- after body fluid exposure risk
- after touching a patient
- after touching a patient’s immediate surroundings
Some additional examples of hand hygiene moments include but are not limited to:
- before handling medication
- before preparing food
- before donning (putting on) and after doffing (taking off) PPE
- after visiting the toilet
- between carrying out different care activities on the same patient
- after cleaning and disinfection procedures
- after handling waste
Download and print the 5 moments of hand hygiene poster.
Wash hands with non-antimicrobial liquid soap and water if:
- hands are visibly soiled or dirty
- hands are potentially contaminated with blood, other body fluids or excretions
- caring for patients with vomiting or diarrhoeal illnesses
- caring for a patient with a suspected or known gastro-intestinal infection, for example Norovirus or a spore forming organism such as Clostridioides difficile
Hands should be washed with warm/tepid water to mitigate the risk of dermatitis associated with repeated exposures to hot water and to maximise hand washing compliance. Compliance may be compromised where water is too hot or too cold. Hands should be dried thoroughly following hand washing using a soft, absorbent, disposable paper towel from a dispenser which is located close to the sink but beyond the risk of splash contamination.
In all other circumstances use hand rub for routine hand hygiene during care.
Staff working in the community should carry a supply of hand rub to enable them to perform hand hygiene at the appropriate times.
Where staff are required to wash their hands in the service user’s own home they should do so for at least 20 seconds using any hand soap available.
Staff should carry a supply of disposable paper towels for hand drying rather than using hand towels in the individual’s own home. Once hands have been thoroughly dried, hand rub should be used.
The use of antimicrobial hand wipes is only permitted where there is no access to running water. Staff must perform hand hygiene using hand rub immediately after using the hand wipes and perform hand hygiene with soap and water at the first available opportunity.
Resources
(The video above demonstrating Hand Washing and Drying Technique was produced by NHS Ayrshire and Arran)
For how to:
- wash hands see Appendix 1
- hand rub see Appendix 2
Hand hygiene posters and leaflets can be found at Wash Your Hands of Them Resources.
NSS supported WHO World Hand Hygiene Day 2024 - Sharing your knowledge about hand hygiene.
Skin care
- Hand rubs when used for hand hygiene should contain emollients in their formulation.
- Warm/tepid water should be used to reduce the risk of dermatitis. Hot water should be avoided.
- Pat hands dry thoroughly after hand washing using disposable paper towels. Avoid rubbing which may lead to skin irritation/damage.
- Use an emollient hand cream during work and when off duty. These should be applied all over the hands including between the fingers and the back of the hands.
- Do not use refillable dispensers or provide communal tubs of hand cream in the care setting.
- Staff with skin problems should seek advice from occupational health or their GP.
- Barrier creams should not be used in the workplace.
Surgical hand antisepsis
Surgical scrubbing/rubbing applies to persons undertaking surgical and some invasive procedures.
Perform surgical scrubbing/rubbing before donning sterile theatre garments or at other times, for example prior to insertion of central vascular access devices.
Surgical scrubbing using an antimicrobial surgical scrub product should be used for the first surgical hand antisepsis of the day. Or perform hand hygiene using water and a non-antimicrobial liquid soap prior to the first surgical antisepsis of the day, this can be carried out in an adjacent clinical area.
For surgical scrubbing
- Remove all hand/wrist jewellery.
- Nail brushes should not be used for surgical hand antisepsis.
- Nail picks (single-use) can be used if nails are visibly dirty.
- Soft, non-abrasive, sterile (single-use) sponges may be used to apply antimicrobial liquid soap to the skin if licensed for this purpose.
- Use an antimicrobial liquid soap licensed for surgical scrubbing or hand rub licensed for surgical rubbing (as specified on the product label).
- Hand rub can be used between surgical procedures if licensed for this use or between glove changes if hands are not visibly soiled.
- Skin should be blotted dry with sterile single-use towels.
Resources
- For surgical scrubbing technique see Appendix 3.
- For surgical rubbing technique see Appendix 4.
Further information can be found in the Hand Hygiene literature reviews:
- Hand washing, hand rubbing and indications for hand hygiene
- Hand hygiene products
- Skin care
- Surgical hand antisepsis in the clinical setting
1.3 Respiratory and Cough Hygiene
 Respiratory and cough hygiene is designed to minimise the risk of cross-transmission of respiratory illness (pathogens).
Respiratory and cough hygiene is designed to minimise the risk of cross-transmission of respiratory illness (pathogens).
- Cover the nose and mouth with a disposable tissue when sneezing, coughing, wiping and blowing the nose. If a disposable tissue is not available use elbow to cover the nose and mouth when coughing or sneezing.
- Patients showing symptoms of respiratory illness should be encouraged to wear a surgical (TYPE II R FRSM) face mask where it is clinically safe and tolerated by the wearer.
- Dispose of used tissues and face masks promptly into a waste bin.
- In the absence of disposable tissues and hand hygiene facilities only, individuals should cough or sneeze into their elbow/sleeve.
- Wash hands with non-antimicrobial liquid soap and warm water after coughing, sneezing, using tissues, or after contact with respiratory secretions or objects contaminated by these secretions.
- Where there is no running water available or hand hygiene facilities are lacking, staff may use hand wipes followed by ABHR and should wash their hands at the first available opportunity.
- Keep contaminated hands away from the eyes nose and mouth.
Staff should promote respiratory and cough hygiene helping those who need assistance with this, for example elderly and children, providing patients with tissues, plastic bags for used tissues and hand hygiene facilities as necessary.
Resources
Further information can be found in the cough etiquette/respiratory hygiene literature review.
1.4 Personal Protective Equipment
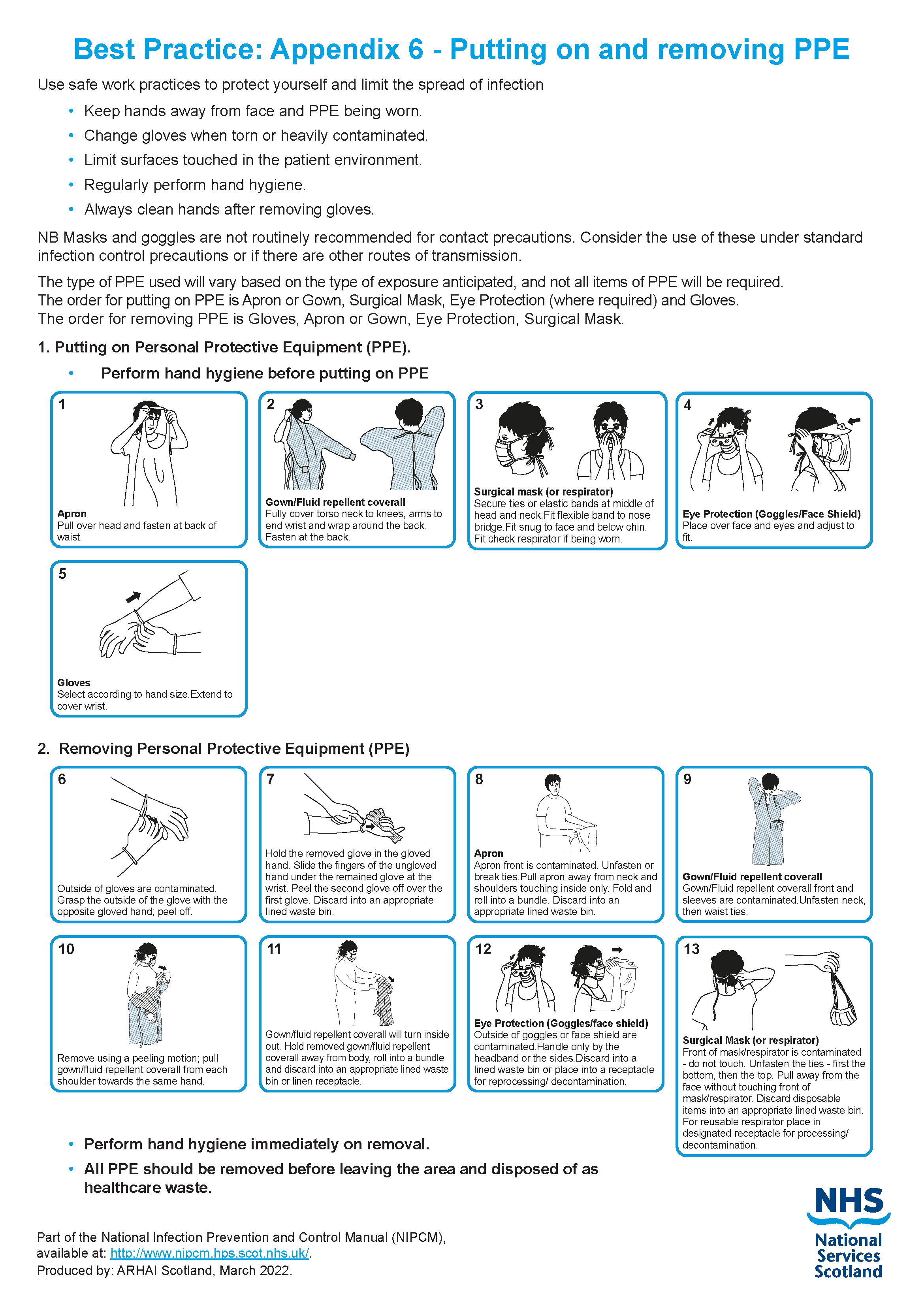
 Before undertaking any care task or procedure staff should assess any likely exposure to blood and/or body fluids and ensure PPE is worn that provides adequate protection against the risks associated with the procedure or task being undertaken.
Before undertaking any care task or procedure staff should assess any likely exposure to blood and/or body fluids and ensure PPE is worn that provides adequate protection against the risks associated with the procedure or task being undertaken.
All PPE should be:
- located close to the point of use
- stored to prevent contamination in a clean/dry area until required for use (expiry dates must be adhered to)
- single-use only items unless specified by the manufacturer
- changed immediately after each patient and/or following completion of a procedure or task
- disposed of after use into the correct waste stream i.e. healthcare waste or domestic waste
Reusable PPE items, for example non-disposable goggles/face shields/visors must have a decontamination schedule with responsibility assigned.
Resources
Further information on best practice for PPE use for SICPs can be found in Appendix 16.
Gloves must:
- be worn when exposure to blood, body fluids, (including but not limited to secretions and/or excretions), non-intact skin, lesions and/or vesicles, mucous membranes, hazardous drugs and chemicals, for example cleaning agents is anticipated/likely. (Scottish National Blood Transfusion Service (SNBTS) adopt practices that differ from those stated in the National Infection Prevention and Control Manual);
- Gloves are a single-use item and should be donned immediately prior to exposure risk and should be changed immediately after each use or upon completion of a task;
- never be worn inappropriately in situations such as to go between patients, move around a care area, work at IT workstations
- be changed if a perforation or puncture is suspected or identified
- be appropriate for use, fit for purpose and well-fitting
- not be worn as a substitute to hand hygiene.
Double gloving is only recommended during some Exposure Prone Procedures (EPPs) e.g. orthopaedic and gynaecological operations or when attending major trauma incidents and when caring for a patient with a suspected or known High Consequence Infectious disease. Double gloving is not necessary at any other time.
Resources
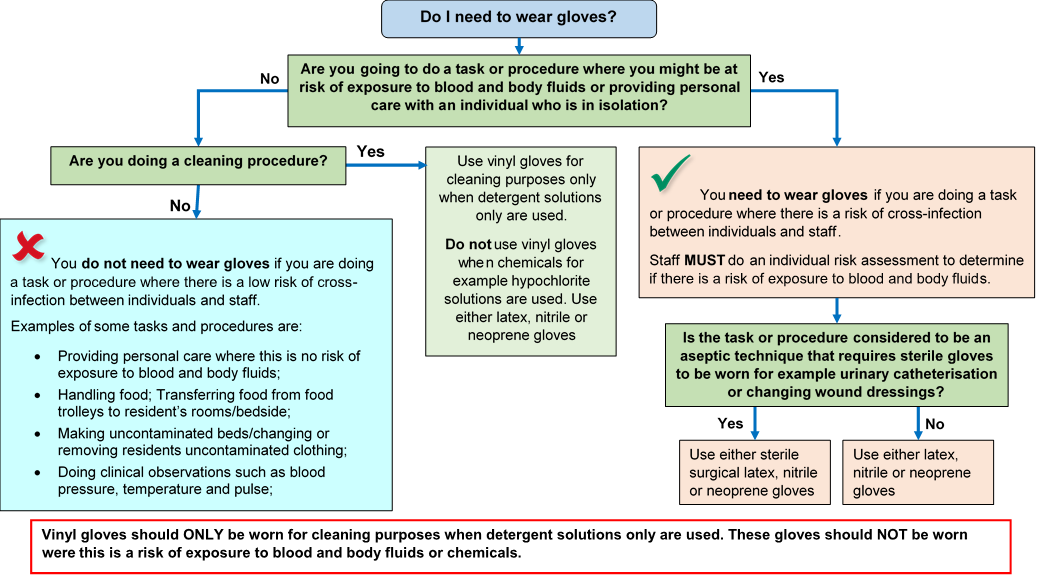
For appropriate glove use and selection see Appendix 5.
Further information can be found in the Gloves literature review.
Aprons must be:
- worn to protect uniform or clothes when contamination is anticipated/likely
- worn when in direct care contact with a patient or their immediate environment, for example providing toileting support or changing bed linen
- changed between patients and following completion of a procedure or task
Full body gowns/fluid repellent coveralls must be:
- worn when there is a risk of extensive splashing of blood and/or other body fluids, for example in the operating theatre
- worn when a disposable apron provides inadequate cover for the procedure/task being performed
- changed between patients and immediately after completion of a procedure or task
The choice of apron or gown is based on a risk assessment and anticipated level of body fluid exposure. Routine sessional use of gowns/aprons is not permitted.
Sterile surgical gowns must be:
- worn by all scrubbed members of the operating theatre surgical team
- worn for insertion of central venous catheters, insertion of peripherally inserted central catheters, insertion of pulmonary artery catheters and spinal, epidural and caudal procedures
Reusable gowns must:
- not be worn in the operating theatre environment or for aseptic surgical procedures
- be appropriately processed between uses based on manufacturer’s instructions
If hand hygiene with soap and water is required, this should not be performed whilst wearing an apron/gown in line with a risk of apron/gown contamination; hand hygiene using ABHR is acceptable.
Resources
Further information can be found in the Aprons/Gowns literature review.
Eye/face protection must:
- be worn if blood and/or body fluid contamination to the eyes/face is anticipated/likely and always during Aerosol Generating Procedures
- be worn by all scrubbed members of the surgical team for all surgical procedures
- not be impeded by accessories such as piercings/false eyelashes
- not be touched when worn
- cover the full peri-orbital region and wrap around the sides of the face
- be removed or changed in accordance with manufacturer’s instructions, if vision is compromised through contamination with blood or body fluids, if the integrity of the equipment is compromised, at the end of a clinical procedure/task and/or prior to leaving the dedicated clinical area.
Regular corrective spectacles and safety spectacles are not considered eye protection.
Resources
Further information can be found in the eye/face protection literature review.
Fluid Resistant Type IIR surgical face masks must be:
- worn by a patient known or suspected to be infected with a micro-organism spread by the droplet or airborne route when leaving their room or when moving between clinical areas including transfers by portering staff and ambulance services
- worn if splashing or spraying of blood, body fluids, secretions or excretions onto the respiratory mucosa (nose and mouth) is anticipated/likely. (As part of SICPs a full-face visor may be used as an alternative to fluid resistant Type IIR surgical face masks to protect against splash or spray)
- worn in combination with a full-face shield, integrated half face shield or goggles for AGPs on non-infectious patients
- worn to protect patients from the operator as a source of infection when performing invasive spinal procedures such as myelography, lumbar puncture and spinal anaesthesia, inserting a Central Vascular Catheter (CVC), performing intra-articular (joint) injections
- worn by all scrubbed members of the theatre surgical team for all surgical procedures
- worn by non-scrubbed members of the theatre surgical team if deemed necessary following a risk assessment of exposure to blood and/or body fluids
- well fitting and fit for purpose (fully covering the mouth and nose)
- removed or changed:
- at the end of a procedure/task
- if the integrity of the mask is breached, e.g. from moisture build-up after prolonged use or from gross contamination with blood or body fluids
- in accordance with specific manufacturers’ instructions
Transparent face masks
Transparent face masks may be used to aide communication with patients in some settings.
Transparent face masks must:
- meet the specification standards of the Transparent face mask technical specification
and
- have been approved by the UK Transparent Mask review group for use within health and social care settings
- only be worn in areas where Fluid Resistant Type IIR surgical face masks are used as personal protective equipment.
Resources
Further information can be found in:
- aerosol generating procedures literature review
- surgical face masks literature review
- section 2.4 of the NIPCM
- appendix 11 of the NIPCM
Footwear must be:
- non-slip, impervious, clean and well maintained, and support and cover the entire foot to avoid contamination with blood or other body fluids or potential injury from sharps
- removed before leaving a care area where dedicated footwear is used, for example theatre. Employees must clean and decontaminate footwear upon removal and when visibly soiled with blood and/or body fluids following manufacturers recommended instructions for cleaning and disinfection
- dedicated for use in settings such as theatres and stored in a designated area when not in use
Footwear found to be defective should be repaired or replaced before further use.
Overshoes/shoe covers should not be used in the general health and care environment.
Resources
Further information can be found in the footwear literature review.
Headwear must be:
- worn in theatre settings/restricted and semi-restricted areas
- worn as PPE for procedures where splashing/spraying of body fluids is anticipated, and as source control when performing clean/aseptic procedures where risk of infection is deemed to be high
- well-fitting and completely cover the hair
- changed/disposed of at the end of a single clinical procedure/task or at the end of a theatre session (for sessional use): immediately if contaminated with blood and/or body fluids
- removed before leaving the theatre/clean room.
Resources
Further information can be found in the headwear literature review
For the recommended method of putting on and removing PPE see video below and Appendix 6.
The correct order for donning, doffing and disposal of PPE for healthcare workers from NHS National Services Scotland on Vimeo.
PPE for visitors
PPE may be offered to visitors to protect them from acquiring a transmissible infection. If a visitor declines to wear PPE when it is offered then this should be respected and the visit must not be refused. PPE use by visitors cannot be enforced and there is no expectation that staff monitor PPE use amongst visitors. Below is the PPE which should be worn where it is appropriate to do so and when the visitor chooses to do so.
Visitors do not routinely require PPE unless they are providing direct care to the individual they are visiting.
The table below provides a guide to PPE for use by visitors if delivering direct care.
IPC Precaution |
Gloves |
Apron |
Face covering/mask |
Eye/Face Protection |
|---|---|---|---|---|
|
Standard Infection Control Precautions (SICPs) |
Not required*1 |
Not required*2 |
Where splash/spray to nose/mouth is anticipated during direct care |
Not required*3 |
|
Transmission Based Precautions (TBPs) |
Not required*1 |
Not required*2 |
If within 2 metres of service user with suspected or known respiratory infection |
If within 2 metres of service user with suspected or known respiratory infection |
*1 unless providing direct care which may expose the visitor to blood and/or body fluids i.e. toileting.
*2 unless providing care resulting in direct contact with the service user, their environment or blood and/or body fluid exposure i.e. toileting, bed bath.
*3 Unless providing direct care and splashing/spraying is anticipated
1.5 Safe Management of Care Equipment

Care equipment is easily contaminated with blood, other body fluids, secretions, excretions and infectious agents. Consequently it is easy to transfer infectious agents from communal care equipment during care delivery.
Care equipment is classified as either:
- Single-use – equipment which is used once on a single patient and then discarded. Must never be reused even on the same patient. The packaging carries the symbol below.

- Needles and syringes are single use devices. They should never be used for more than one patient or reused to draw up additional medication.
- Never administer medications from a single-dose vial or intravenous (IV) bag to multiple patients.
- Single patient use – equipment which can be reused on the same patient.
- Reusable invasive equipment - used once then decontaminated for example surgical instruments.
- Reusable non-invasive equipment (often referred to as communal equipment) - reused on more than one patient following decontamination between each use e.g. commode, patient transfer trolley.
Before using any sterile equipment check that:
- the packaging is intact
- there are no obvious signs of packaging contamination
- the expiry date remains valid
Decontamination of reusable non-invasive care equipment must be undertaken:
- between each use
- after blood and/or body fluid contamination
- at regular predefined intervals as part of an equipment cleaning protocol
- before inspection, servicing or repair
Adhere to manufacturers’ guidance for use and decontamination of all care equipment.
All reusable non-invasive care equipment must be rinsed and dried following decontamination then stored clean and dry.
Decontamination protocols should include responsibility for, frequency of and method of environmental decontamination.
An equipment decontamination status certificate will be required if any item of equipment is being sent to a third-party, for example for inspection, servicing or repair.
Guidance may be required prior to procuring, trialling or lending any reusable non-invasive equipment.
Resources
Further information can be found in the management of care equipment literature review.
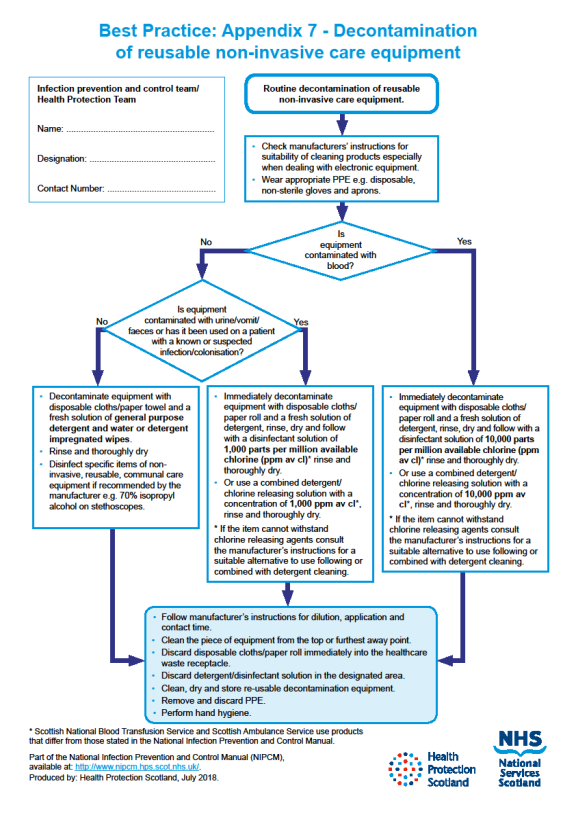
For how to decontaminate reusable non-invasive care equipment see Appendix 7.
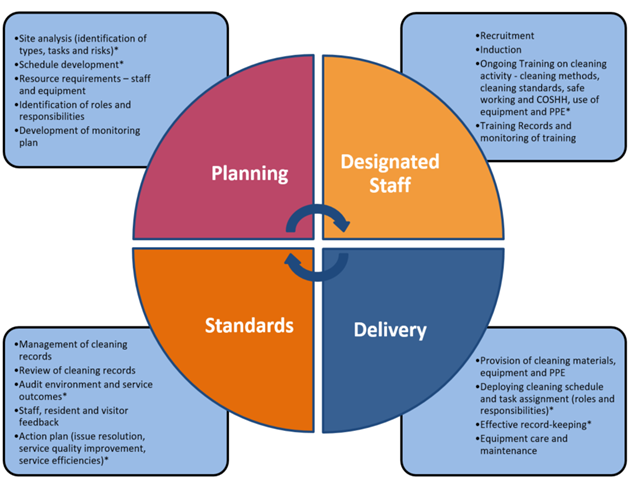
1.6 Safe Management of Care Environment
 It is the responsibility of the person in charge to ensure that the care environment is safe for practice (this includes environmental cleanliness/maintenance). The person in charge must act if this is deficient.
It is the responsibility of the person in charge to ensure that the care environment is safe for practice (this includes environmental cleanliness/maintenance). The person in charge must act if this is deficient.
The care environment must be:
- visibly clean, free from non-essential items and equipment to facilitate effective cleaning
- well maintained and in a good state of repair
- routinely cleaned in accordance with the Health Facilities Scotland (HFS) National Cleaning Specification:
- a fresh solution of general-purpose neutral detergent in warm water is recommended for routine cleaning. This should be changed when dirty or at 15 minutes intervals or when changing tasks
- routine disinfection of the environment is not recommended. However, 1,000ppm available chlorine should be used routinely on sanitary fittings
Staff groups should be aware of their environmental cleaning schedules and clear on their specific responsibilities.
Cleaning protocols should include responsibility for; frequency of; and method of environmental decontamination.
When an organisation adopts decontamination processes not recommended in the NIPCM the care organisation is responsible for governance of and completion of local risk assessment(s) to ensure safe systems of work.
Resources
Further information can be found in the routine cleaning of the environment in hospital setting literature review.
1.7 Safe Management of Linen
 Clean linen
Clean linen
- Should be stored in a clean, designated area, preferably an enclosed cupboard.
- If clean linen is not stored in a cupboard then the trolley used for storage must be designated for this purpose and completely covered with an impervious covering that is able to withstand decontamination.
Linen used during patient transfer
- Any linen used during patient transfer, for example blankets, should be categorised at the point of destination.
For all used linen (previously known as soiled linen)
- Ensure a laundry receptacle is available as close as possible to the point of use for immediate linen deposit.
- Do not:
- rinse, shake or sort linen on removal from beds/trolleys
- place used linen on the floor or any other surfaces, for example a locker/table top
- re-handle used linen once bagged
- overfill laundry receptacles
- place inappropriate items in the laundry receptacle, for example used equipment/needles
For all infectious linen (this mainly applies to healthcare linen)
This is linen that has been used by a patient who is known or suspected to be infectious and/or linen that is contaminated with blood and/or other body fluids for example faeces.
- Place directly into a water-soluble/alginate bag and secure, then place into a plastic bag, for example clear bag, and secure before placing in a laundry receptacle. This applies also to any item(s) heavily soiled and unlikely to be fit for reuse.
- Used and infectious linen bags/receptacles must be tagged, for example ward/care area and date.
- Store all used/infectious linen in a designated, safe, lockable area whilst awaiting uplift. Uplift schedules must be acceptable to the care area and there should be no build-up of linen receptacles.
Local guidance regarding management of linen may be available.
All linen that is deemed unfit for re-use, for example torn or heavily contaminated, should be categorised at the point of use and returned to the laundry for disposal.
Resources
Further information can be found in the safe management of linen literature review and National Guidance for Safe Management of Linen in NHSScotland Health and Care Environments - For laundry services/distribution.
Further information about linen bagging and tagging can be found in Appendix 8.
Scottish Government uniform, dress code and laundering policy is available.
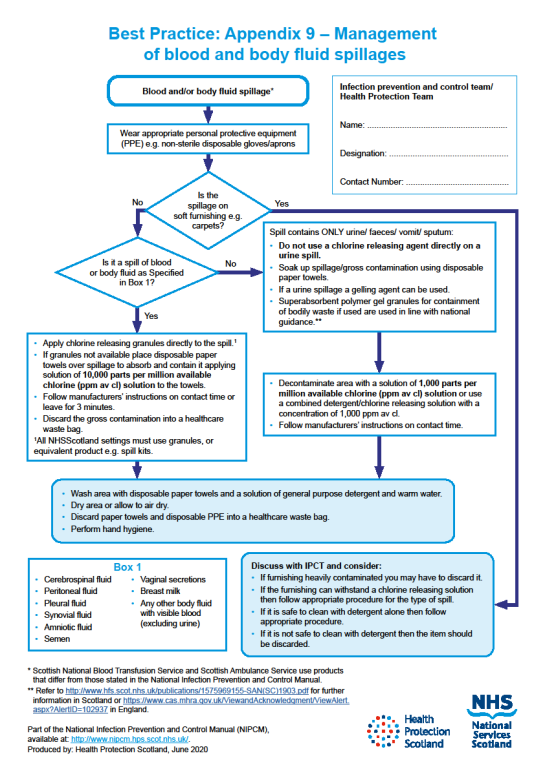
1.8 Safe Management of Blood and Body Fluid Spillages
 Spillages of blood and other body fluids may transmit blood borne viruses.
Spillages of blood and other body fluids may transmit blood borne viruses.
Spillages must be decontaminated immediately by staff trained to undertake this safely.
Responsibilities for the decontamination of blood and body fluid spillages should be clear within each area/care setting.
If superabsorbent polymer gel granules for containment of bodily waste are used these should be used in line with national guidance. In Scotland refer to Safety Action Notice - SAN(SC)19/03 | National Services Scotland (nhs.scot)
Resources
For management of blood and body fluid spillages see Appendix 9.
Further information can be found in the management of blood and body fluid in health and social care settings literature review.
1.9 Safe Disposal of Waste (including sharps)
 Scottish Health Technical Note (SHTN) 3: NHSScotland Waste Management Guidance contains the regulatory waste management guidance for NHSScotland including waste classification, segregation, storage, packaging, transport, treatment and disposal.
Scottish Health Technical Note (SHTN) 3: NHSScotland Waste Management Guidance contains the regulatory waste management guidance for NHSScotland including waste classification, segregation, storage, packaging, transport, treatment and disposal.
The Health and Safety (Sharp Instruments in Healthcare) Regulations 2013 outline the regulatory requirements for employers and contractors in the healthcare sector in relation to the safe disposal of sharps.
Categories of waste
- Healthcare (including clinical) waste – is produced as a direct result of healthcare activities, for example soiled dressings, sharps.
- Special (or hazardous) waste – arises from the delivery of healthcare in both clinical and non-clinical settings. Special waste includes a range of controlled wastes, defined by legislation, which contain dangerous or hazardous substances for example chemicals, pharmaceuticals.
- Domestic waste – must be segregated at source into:
- dry recyclates (glass, paper and plastics, metals, cardboard)
- residual waste (any other domestic waste that cannot be recycled).
Waste streams
- Black – trivial risk
- Domestic waste or yellow and black stripes (small quantities of hygiene waste).
- Final disposal to landfill.
- Clear/opaque receptacles may also be used for domestic waste at care area level.
- Orange, light blue (laboratory) – low risk
- Orange - consists of items which are contaminated or likely to be contaminated with blood and/or body fluids including saliva. Final disposal following heat disinfection is to landfill.
- Light blue – laboratory/microbiological waste that must be autoclaved before disposal via the orange stream.
- Yellow– high risk
- Waste which poses ethical, highly infectious or contamination risks.
- This includes anatomical and human tissue which is recognisable as body parts, medical devices and sharps waste boxes that have red, purple or blue lids.
- Disposal is by specialist incineration.
- Red – special waste
- Chemical waste.
For care/residential homes waste disposal may differ from the categories described above and guidance from local contractors will apply. Refer to SEPA guidance.
Safe waste disposal at care area level
Always dispose of waste:
- immediately and as close to the point of use as possible
- into the correct segregated colour coded UN 3291 approved waste bag (either orange/yellow for healthcare waste or black/clear/opaque for domestic) or container (sharps box)
Liquid waste, for example blood, must be rendered safe by adding a self-setting gel or compound before placing in an orange lidded leak-proof bin.
Waste bags must be no more than 3/4 full or more than 4 kgs in weight and use a ratchet tag/or tape (for healthcare waste bags only) using a ‘swan neck’ to close with the point of origin and date of closure clearly marked on the tape/tag.
Store all waste in a designated, safe, lockable area whilst awaiting uplift. Uplift schedules must be acceptable to the care area and there should be no build-up of waste receptacles.
Sharps boxes must:
- have a dedicated handle
- have a temporary closure mechanism, which must be employed when the box is not in use
- be labelled with date of assembly, point of origin and date of closure.
- be disposed of when the manufacturers’ fill line is reached or following 3 months of assembly (whichever is first)
Local guidance regarding management of waste at care level may be available.
Resources
Further information can be found in the safe disposal of waste literature review.
1.10 Occupational Safety: Prevention and Exposure Management (including sharps)
 Exposure in relation to blood borne viruses (BBV) is the focus within this section and reflects the existing evidence base.
Exposure in relation to blood borne viruses (BBV) is the focus within this section and reflects the existing evidence base.
The Health and Safety (Sharp Instruments in Healthcare) Regulations 2013 outline the regulatory requirements for employers and contractors in the healthcare sector in relation to:
- arrangements for the safe use and disposal of sharps
- provision of information and training to employees
- investigations and actions required in response to work related sharps injuries
Sharps handling must be assessed, kept to a minimum and eliminated if possible with the use of approved safety devices.
Manufacturers’ instructions for safe use and disposal must be followed.
Needles must not be re-sheathed/recapped.4
Always dispose of needles and syringes as 1 unit.
If a safety device is being used safety mechanisms must be deployed before disposal.
Occupational exposure
An occupational exposure is a percutaneous or mucocutaneous exposure to blood or other body fluids.
Occupational exposure risk can be reduced via application of other SICPs and TBPs outlined within the NIPCM.
Significant occupational exposure
A significant occupational exposure is a percutaneous or mucocutaneous exposure to blood or other body fluids from a source that is known, or found to be positive for a blood borne virus (BBV).
Examples of significant occupational exposures would be:
- a percutaneous injury, for example injuries from needles, instruments, bone fragments, or bites which break the skin
- exposure of broken skin, for example abrasions, cuts, eczema
- exposure of mucous membranes including the eye from splashing of blood or other high risk body fluids
There is a potential risk of transmission of a Blood Borne Virus (BBV) from a significant occupational exposure and staff must understand the actions they should take when a significant occupational exposure incident takes place. There is a legal requirement to report all sharps injuries and near misses to line managers/employers.
Additionally, employers are obligated to minimise or eliminate workplace risks where it is reasonably practicable. Immunisation against BBV should be available to all qualifying staff, and testing (and post exposure prophylaxis when applicable) offered after significant occupational exposure incidents.
Resources
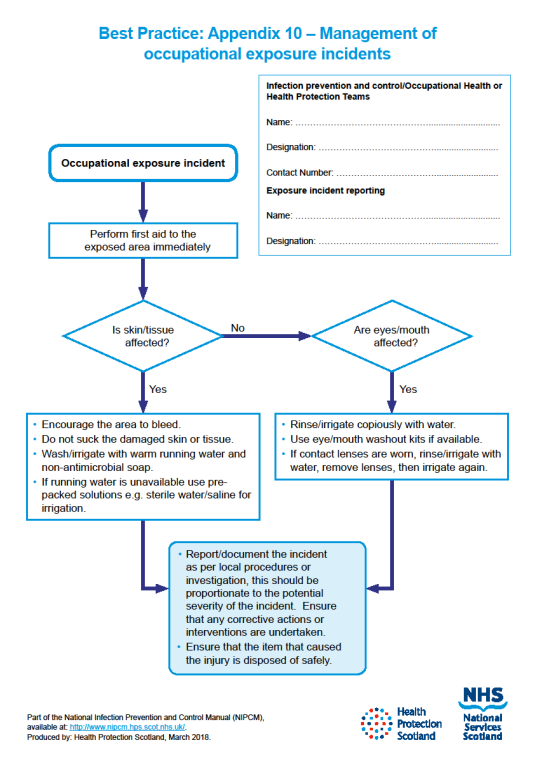
For the management of an occupational exposure incidents see Appendix 10
Exposure prone procedures (EEPs)
Exposure prone procedures (EEPs) are invasive procedures where there is a risk that injury to the healthcare worker may result in the exposure of the patient’s open tissues to the blood of the worker (bleed-back).
There are some exclusions for HCWs with known BBV infection when undertaking EPPs. The details of these and further information can be found in the occupational exposure management (including sharps) literature review.
4 A local risk assessment is required if re-sheathing is undertaken using a safe technique for example anaesthetic administration in dentistry.
Chapter 2 - Transmission Based Precautions (TBPs)
SICPs may be insufficient to prevent cross transmission of specific infectious agents. Therefore, additional precautions, TBPs, are required to be used by staff when caring for patients with a known or suspected infection or colonisation.
Clinical judgement and decisions should be made by staff on the necessary precautions. This must be based on the:
- suspected or known infectious agent
- transmission route of the infectious agent
- care setting and procedures undertaken
- severity of the illness caused
TBPs are categorised by the route of transmission of infectious agents (some infectious agents can be transmitted by more than one route): Appendix 11 provides details of the type of precautions, optimal patient placement, isolation requirements and any respiratory precautions required. Application of TBPs may differ depending on the setting and the known or suspected infectious agent.
Please Note: The Transmission Based Precautions Literature Review is currently undergoing a full update with new research questions (available on request).
Contact precautions
Used to prevent and control infections that spread via direct contact with the patient or indirectly from the patient’s immediate care environment (including care equipment). This is the most common route of cross-infection transmission.
Droplet precautions
Used to prevent and control infections spread over short distances (at least 3 feet or 1 metre) via droplets (greater than 5μm) from the respiratory tract of one individual directly onto a mucosal surface or conjunctivae of another individual. Droplets penetrate the respiratory system to above the alveolar level.
Airborne precautions
Used to prevent and control infections spread without necessarily having close patient contact via aerosols (less than or equal to 5μm) from the respiratory tract of one individual directly onto a mucosal surface or conjunctivae of another individual. Aerosols penetrate the respiratory system to the alveolar level.
Further information on Transmission Based Precautions can be found in the definitions of Transmission Based Precautions literature reviews.
Last updated: 28 August 2023
2.1 Patient Placement/Assessment for Infection Risk
The potential for transmission of infection must be assessed at the patient’s entry to the care area. If hospitalised or in a care home setting this should be continuously reviewed throughout the stay/period of care. The assessment should influence placement decisions in accordance with clinical/care need(s).
Patients who may present a cross-infection risk in any setting includes but is not limited to those:
- with symptoms such as loose stools or diarrhoea, vomiting, fever or respiratory symptoms.
- with a known (laboratory confirmed) or suspected infectious pathogen for which appropriate duration of precautions as outlined in A-Z of pathogens are not yet complete
- known or suspected to have been previously positive with a Multi-drug Resistant Organism (MDRO), for example MRSA, CPE
- who have been hospitalised (inpatient) outside Scotland in the last 12 months (including those who received dialysis)
Further information regarding general respiratory screening questions can be found within the resources section of the NIPCM.
Isolation facilities should be prioritised depending on the known/suspected infectious agent (refer to Aide Memoire - Appendix 11). All patient placement decisions and assessment of infection risk (including isolation requirements) must be clearly documented in the patient notes.
When single-bed rooms are limited, patients who have conditions that facilitate the transmission of infection to other patients (e.g., draining wounds, stool incontinence, uncontained secretions) and those who are at increased risk of acquisition and adverse outcomes resulting from HAI (e.g., immunosuppression, open wounds, invasive devices, anticipated prolonged length of stay, total dependence on HCWs for activities of daily living) should be prioritised for placement in a single-bed room. Single-bed room prioritisation should be reviewed daily and the clinical judgement and expertise of the staff involved in a patient's management and the Infection Prevention and Control Team (IPCT) or Health Protection Team (HPT) should be sought particularly for the application of TBPs e.g. isolation prioritisation when single rooms are in short supply.
Hospital settings
- Patients who present a cross-infection risk should be isolated in a single room or for patients with a known or suspected pathogen spread by the airborne route, in a specialised negative pressure isolation facility where available.
- Isolation of infectious patients can be in specialised isolation facilities, single room isolation, cohorting of infectious patients where appropriate, ensuring that they are separated by at least 2 metres with the door closed.
- Signage should be used on doors/areas to communicate isolation requirements and prevent entry of unnecessary visitors and non-essential staff.
- Infectious patients should only be transferred to other departments if medically necessary. If the patient has an infectious agent transmitted by the airborne/droplet route, then if possible/tolerated the patient should wear a surgical face mask during transfer.
- Receiving department/hospital and transporting staff must be aware of the necessary precautions.
Cohorting in hospital settings
Cohorting of patients
Cohorting of patients should only be considered when single rooms are in short supply and should be undertaken in conjunction with the local IPCT.
Patients who should not be placed in multi bed cohorts:
- patients with different infectious pathogens/strains and patients with unknown infectious pathogens (laboratory confirmation still awaited)
- patients considered more vulnerable to infection
- patients with a known or suspected infectious pathogen spread by the droplet/airborne route who will undergo an AGP
- patients who are unlikely to comply with TBPs
Staff cohorting
Consider assigning a dedicated team of care staff to care for patients in isolation/cohort rooms/areas as an additional infection control measure during outbreaks/incidents. This can only be implemented through planning of staff rotas if there are sufficient levels of staff available to ensure consistency in staff allocation (so as not to have a negative impact on non-affected patients’ care).
Before discontinuing isolation in hospital settings
Individual patient risk factors should be considered, for example there may be prolonged shedding of certain microorganisms in immunocompromised patients). Clinical and molecular tests to show the absence of microorganisms may be considered in the decision to discontinue isolation and can reduce isolation times. The clinical judgement and expertise of the staff involved in a patient’s management and the Infection Prevention and Control Team (IPCT) or Health Protection Team (HPT) should be sought on decisions regarding isolation discontinuation.
Primary care/out-patient settings
- Patients attending these settings with suspected/known infection/colonisation should be prioritised for assessment/treatment, for example scheduled appointments at the start or end of the clinic session. Infectious patients should be separated from other patients whilst awaiting assessment and during care management wherever possible.
- If transfer from a primary care facility to hospital is required, the ambulance service should be informed of the infectious status of the patient.
Resources
Further information can be found in the patient placement literature review.
2.2 Safe Management of Patient Care Equipment in an Isolation Room/Cohort Area
- Use single-use items if possible.
- Reusable non-invasive care equipment should be dedicated to the isolation room/cohort area and decontaminated prior to use on another patient Section 1.5. Safe Management of Care Equipment
- An increased frequency of decontamination should be considered for reusable non-invasive care equipment when used in isolation/cohort areas.
If an item cannot withstand chlorine releasing agents staff are advised to consult the manufacturer’s instructions for a suitable alternative to use following or combined with detergent cleaning.
Resources
For how to decontaminate non-invasive reusable equipment see Appendix 7.
Note: Scottish Ambulance Service (SAS) and Scottish National Blood Transfusion Service adopt practices that differ from those stated in the National Infection Prevention and Control Manual.
2.3 Safe Management of the Care Environment
Routine environmental decontamination
Hospital/care home setting
Patient isolation/cohort rooms/area must be decontaminated at least daily, this may be increased on the advice of IPCTs/HPTs. These areas must be decontaminated using either:
- a combined detergent/disinfectant solution at a dilution of 1,000 parts per million available chlorine (ppm available chlorine (av.cl.)) or
- a general purpose neutral detergent in a solution of warm water followed by disinfection solution of 1,000ppm av.cl.
Manufacturers’ guidance and recommended product "contact time" must be followed for all cleaning/disinfection solutions .
Increased frequency of decontamination/cleaning schedules should be incorporated into the environmental decontamination schedules for areas where there may be higher environmental contamination rates, for example
- toilets/commodes particularly if patients have diarrhoea
- “frequently touched” surfaces such as door/toilet handles and locker tops, over bed tables and bed rails
Patient rooms must be terminally cleaned following resolution of symptoms, discharge or transfer. This includes removal and laundering of all curtains and bed screens.
Vacated rooms should also be decontaminated following an AGP.
Primary care/out-patient settings
The extent of decontamination between patients will depend on the duration of the consultation/assessment, the patients presenting symptoms and any visible environmental contamination.
Equipment used for environmental decontamination must be either single-use or dedicated to the affected area then decontaminated or disposed of following use for example cloths, mop heads.
Terminal decontamination
Following patient transfer, discharge, or once the patient is no longer considered infectious.
Remove from the vacated isolation room/cohort area, all:
- healthcare waste and any other disposable items (bagged before removal from the room)
- bedding/bed screens/curtains and manage as infectious linen (bagged before removal from the room)
- reusable non-invasive care equipment (decontaminated in the room prior to removal) Appendix 7.
The room should be decontaminated using either:
- a combined detergent disinfectant solution at a dilution (1,000ppm av.cl.) or
- a general purpose neutral detergent clean in a solution of warm water followed by disinfection solution of 1,000ppm av.cl..
The room must be cleaned from the highest to lowest point and from the least to most contaminated point.
Manufacturers’ guidance and recommended product "contact time" must be followed for all cleaning/disinfection solutions .
Unless instructed otherwise by the IPCT there is no requirement for a terminal clean of an outpatient area or theatre recovery.
Note: Scottish Ambulance Service (SAS) and Scottish National Blood Transfusion Service adopt practices that differ from those stated in the National Infection Prevention and Control Manual.
When an organisation adopts practices that differ from those recommended/stated in the NIPCM with regards to cleaning agents, the individual organisation is fully responsible for ensuring safe systems of work, including the completion of local risk assessment(s) approved and documented through local governance procedures.
2.4 Personal Protective Equipment (PPE)
2.4.1 Surgical masks
A type IIR fluid resistant surgical mask should be worn when caring for a patient with a suspected/confirmed infectious agent spread by the droplet route.
Surgical masks worn by patients with suspected/confirmed infectious agents spread by the droplet or airborne routes, as a form of source control, should meet type II or IIR standards.
2.4.2 Eye/face protection
A face visor or goggles should be used in combination with a fluid resistant type IIR surgical mask when caring for symptomatic patients infected with droplet transmitted infectious agents.
A face visor or goggles should be used in combination with a fluid resistant FFP3 respirator when caring for symptomatic patients infected with an airborne transmitted infectious agent.
Eye/face protection should be worn
- by all of those in the room when potentially infectious AGPs are conducted
- for the care of patients with novel infectious agents including pandemic influenza
2.4.3 Aprons/Gowns
An apron should be worn when caring for patients known or suspected to be colonised/infected with antibiotic resistant bacteria including contact with the patient’s environment.
Plastic aprons should be used in health and social care settings for protection against contamination with blood and/or body fluids.
A fluid repellent gown should be used if excessive splashing or spraying is anticipated.
A full body fluid repellent gown should be worn when conducting AGPs on patients known or suspected to be infected with a respiratory infectious agent.
Resources
Further information can be found in the Aprons/Gowns literature review.
2.4.4 Gloves
Gloves must:
- be worn when exposure to blood, body fluids, (including but not limited to secretions and/or excretions), non-intact skin, lesions and/or vesicles, mucous membranes, hazardous drugs and chemicals, e.g. cleaning agents is anticipated/likely;2
- Gloves are a single-use item and should be donned immediately prior to exposure risk and should be changed immediately after each use or upon completion of a task;
- never be worn inappropriately in situations such as; to go between patients, move around a care area, work at IT workstations;
- be changed if a perforation or puncture is suspected or identified;
- be appropriate for use, fit for purpose and well-fitting;
- not be worn as a substitute to hand hygiene.
Double gloving is only recommended during some Exposure Prone Procedures (EPPs), for example orthopaedic and gynaecological operations, or when attending major trauma incidents and when caring for a patient with a suspected or known High Consequence Infectious disease. Double gloving is not necessary at any other time.
Resources
For appropriate glove use and selection see Appendix 5.
Further information can be found in the Gloves literature review.
2.4.5 RPE
PPE must still be used in accordance with SICPs when using Respiratory Protective Equipment. See Chapter 1.4 for PPE use for SICPs.
Where it is not reasonably practicable to prevent exposure to a substance hazardous to health (as may be the case where healthcare workers are caring for patients with suspected or known airborne micro-organisms) the hazard must be adequately controlled by applying protection measures appropriate to the activity and consistent with the assessment of risk. If the hazard is unknown the clinical judgement and expertise of IPC/HP staff is crucial and the precautionary principle should apply.
Respiratory Protective Equipment (RPE), for instance FFP3 and facial protection, must be considered when:
- a patient is admitted with a known/suspected infectious agent/disease spread wholly by the airborne route
- carrying out aerosol generating procedures (AGPs) on patients with a known/suspected infectious agent spread wholly or partly by the airborne or droplet route
See Appendix 17 for the extant list of Aerosol Generating Procedures which require the application of airborne precautions. Appendix 17 also includes details of associated Post AGP Fallow times.
Filter Face Piece 3 (FFP3) Respirators
Where staff have concerns, they may choose to wear an FFP3 respirator rather than a fluid-resistant surgical mask (FRSM) when providing patient care, provided they are fit tested. This is a personal PPE risk assessment.
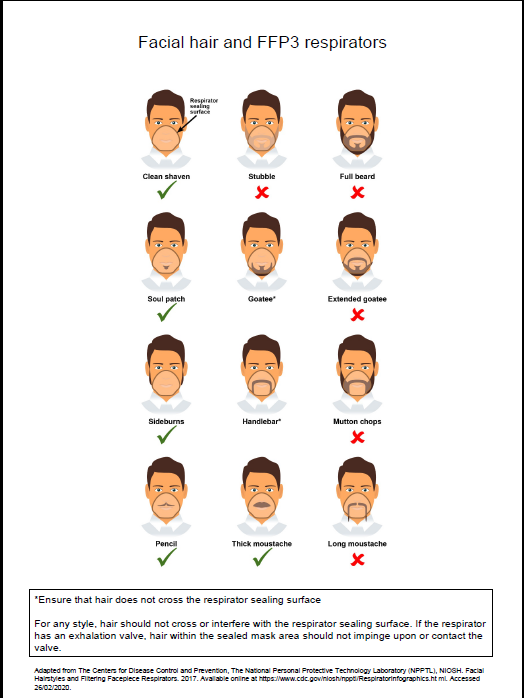
All tight fitting RPE (for instance FFP3) respirators must be:
- fit tested (by a competent fit test operator) on all healthcare staff who may be required to wear a respirator to ensure an adequate seal/fit according to the manufacturers’ guidance
- fit checked (according to the manufacturers’ guidance) every time a respirator is donned to ensure an adequate seal has been achieved. The poster below gives further information on compatibility of facial hair and FFP3 respirators and can be used when fit testing and fit checking
- single use (disposable) and fluid-resistant. Valved respirators may be shrouded or unshrouded. Respirators with unshrouded valves are not considered to be fluid-resistant and therefore should be worn with a full face shield if blood or body fluid splashing is anticipated
- non valved if a sterile procedure is being performed at the same time as an AGP requiring a respirator to be worn. An MHRA safety alert can be viewed.
- compatible with other facial protection used, for instance protective eyewear, so that this does not interfere with the seal of the respiratory protection. Regular corrective spectacles are not considered adequate eye protection. If wearing a valved, non-shrouded FFP3 respirator a full face shield/visor must be worn
- always put on before entry into the patient room/area and prior to performing an aerosol generating procedure (AGP) and removed in an anteroom/lobby or in a safe area, for example outside the isolation/cohort room/area. All other PPE should be removed in the patient care area
- changed after each use. Other indications that a change in respirator is required include: if breathing becomes difficult, if the respirator becomes wet or moist, damaged or obviously contaminated with body fluids such as respiratory secretions.
Resources
Poster on compatibility of facial hair and FFP3 respirators can be used when fit testing and fit checking.
Further information regarding fitting and fit checking of respirators can be found on the Health and Safety Executive website.
National Priority Risk Categorisation for face fit testing with FFP3
The following risk categorisation is the minimum requirement for staff groups that require FFP3 fit testing. NHS boards can add to this for example where high-risk units are present. This categorisation is inclusive of out of hours services.
Level 1 – Preparedness for business as usual
Staff in clinical areas most likely to provide care to patients who present at healthcare facilities with an infectious pathogen spread by the airborne route; and/or undertake aerosol generating procedures. These are A&E, ICU, paediatrics, respiratory, infectious diseases, anaesthesia, theatres, Chest physiotherapists, Special Operations Response Team (Ambulance), A&E Ambulance Staff, Bronchoscopy Staff, Resuscitation teams, mortuary staff.
Level 2 – Preparedness in the event of emerging threat
Staff in clinical setting likely to provide care to patients admitted to hospital in the event of an emerging threat, for example Medical receiving, Surgical, Midwifery and Speciality wards, all other ambulance transport staff.
In the event of an ‘Epidemic/Pandemic’ Local Board Assessment as per their preparedness plans will apply.
The decision to wear an FFP3 respirator/hood should be based on clinical risk assessment, for example task being undertaken, the presenting symptoms, the infectious state of the patient, risk of acquisition and the availability of treatment.
Resources
For a list of organisms spread wholly or partly by the airborne (aerosol) or droplet routes see Appendix 11.
Further information can be found in the aerosol generating procedures literature review.
Powered respirator hoods
Powered respirator hoods are an alternative to FFP3 respirators for example when fit testing cannot be achieved.
Powered hoods must be:
- single use (disposable) and fluid resistant
- the filter must be enclosed with the exterior and the belt able to withstand disinfection with 10,000ppm av.cl.
FFP3 respirator or powered respirator hood
- may be considered for use by visitors if there has been no previous exposure to the infected person or infectious agent; but
- must never be worn by an infectious patient(s) due to the nature of the respirator filtration of incoming air not expelled air.
Work is currently underway by the UK Re-useable Decontamination Group examining the suitability of respirators for decontamination. This literature review will be updated to incorporate recommendations from this group when available. In the interim, ARHAI Scotland are unable to provide assurances on the efficacy of respirator decontamination methods and the use of re-useable respirators is not recommended.
Further information can be found in the Respiratory Protective Equipment (RPE) literature review and the Personal Protective Equipment (PPE) for Infectious Diseases of High Consequence (IDHC) literature review.
Frameworks to support the assessing and recording of staff competency in PPE for HCID are available in the resources section of the NIPCM.
2.5 Infection Prevention and Control during care of the deceased
The principles of SICPs and TBPs continue to apply whilst deceased individuals remain in the care environment. This is due to the ongoing risk of infectious transmission via contact although the risk is usually lower than for living patients.
It is important that information on the infection status of the deceased is sought and communicated at each stage of handling. Appropriate risk assessment must be carried out before performing activities that may increase the risk of transmission of infectious agents from deceased individuals (see literature review for further information on these activities).
Washing and/or dressing should not be carried out when the deceased is known or suspected to have been infected by any of the following key infectious agents: Hazard Group 4 organisms, anthrax, and rabies. For other HCIDs a local risk assessment should be undertaken to inform any decision making on washing and/or dressing of the deceased.
Viewing of the deceased should be avoided when the deceased is known or suspected to have been infected by Hazard Group 4 organisms, specifically those causing VHFs (including Ebola, Lassa etc.) and anthrax. For other HCIDs a local risk assessment should be undertaken to inform any decision making on viewing of the deceased.
See Appendix 12 Application of infection control precautions in the deceased.
Staff should advise relatives of the appropriate precautions when viewing and/or having physical contact with the deceased including when this should be avoided.
Deceased individuals known or suspected to have a Hazard Group 4 infectious agent should be placed in a sealed double plastic body bag with absorbent material placed between each bag. The surface of the outer bag should then be disinfected with 1000 ppm av.cl before being placed in a robust sealed coffin.
Post-mortem examination should not be performed on a deceased individual known or suspected to have Hazard Group 4 infectious agents. See Appendix 12 Application of infection control precautions in the deceased. Blood sampling can be undertaken in the mortuary by a competent person to confirm or exclude this diagnosis. Refer to Section 2.4 for suitable PPE.
Post-mortem examination of deceased individuals known or suspected to have been infected by transmissible spongiform encephalopathies (TSE) causing agents should be carried out in such a way as to minimise contamination of the working environment. See Literature review for further information.
Chapter 3 - Healthcare Infection Incidents, Outbreaks and Data Exceedance
The purpose of this chapter is to support the early recognition of potential infection incidents and to guide IPCT/HPTs in the incident management process within care settings; (that is, NHSScotland, independent contractors providing NHS services and private providers of care).
This guidance is aligned to the Management of Public Health Incidents: Guidance on the Roles and Responsibilities of NHS led Incident Management Teams
Built environment incidents/outbreaks
ARHAI Scotland are currently working towards delivery of comprehensive evidence-based guidance which will form Chapter 4 of the National Infection Prevention and Control Manual (NIPCM) on the built environment and decontamination.
Two Aide-Memoires currently provide best practice recommendations to be implemented in the event of a healthcare water-associated or healthcare ventilation-associated infection incident/outbreak. These will ensure clinical staff, estates and facilities staff, and Infection Prevention and Control Teams (IPCT) have an understanding of the preventative measures required and the appropriate actions that should be taken.
Prevention and management of healthcare water-associated infection incidents/outbreaks
Prevention and management of healthcare ventilation-associated infection incidents/outbreaks
3.1 Definitions of Healthcare Infection Incident, Outbreak and Data Exceedance
The terms ‘incident’ and ‘Incident Management Team’ (IMT) are used as generic terms to cover both incidents and outbreaks
A healthcare infection incident may be:
An exceptional infection episode
- a single case of rare infection that has severe outcomes for an individual AND has major implications for others (patients, staff and/or visitors), the organisation or wider public health for example, high consequence infectious disease (HCID) OR other rare infections such as XDR-TB, botulism, polio, rabies, or diphtheria.
See literature review for Infectious Diseases of High Consequence (IDHC)
A healthcare infection exposure incident
- Exposure of patients, staff, public to a possible infectious agent as a result of a healthcare system failure or a near miss e.g. ventilation, water or decontamination incidents.
A healthcare associated infection outbreak
- Two or more linked cases with the same infectious agent associated with the same healthcare setting over a specified time period.
or
- A higher-than-expected number of cases of HAI in a given healthcare area over a specified time period.
A healthcare infection data exceedance
- A greater than expected rate of infection compared with the usual background rate for the place and time where the incident has occurred.
A healthcare infection near miss incident
- An incident which had the potential to expose patients to an infectious agent but did not e.g. decontamination failure.
A healthcare infection incident should be suspected if there is:
- a single case of an infection for which there have previously been no cases in the facility (e.g. infection with a multidrug-resistant organism (MDRO) with unusual resistance patterns or a post-procedure infection with an unusual organism)
Resources
Further information can be found in the literature review Healthcare infection incidents and outbreaks in Scotland.
3.2 Detection and recognition of a Healthcare Infection incident/outbreak or data exceedance
An early and effective response to an actual or potential healthcare incident, outbreak or data exceedance is crucial. The local Board IPCT and HPT should be aware of and refer to the national minimum list of alert organisms/conditions. See Appendix 13.
Healthcare associated infection (HAI) Surveillance systems should be used to aid incident/outbreak detection using a combination of retrospective detection of cases alongside prospective enhanced surveillance in high-risk settings (ICU/PICU/NICU, oncology/haematology). A risk-based approach should be applied for other vulnerable groups e.g. cystic fibrosis, oncology and those undergoing renal dialysis.
Local surveillance/reporting systems should be used for recognition and detection of potential healthcare infection incidents/outbreaks within NHS boards. Systems should make use of ‘triggers’ to allow prompt detection of any variance from normal limits.
The Infection Prevention & Control Team (IPCT)/Health Protection Team (HPT) should utilise surgical site infection (SSI) surveillance systems to identify specific post-surgical healthcare infection incidents/outbreaks (in line with national SSI surveillance program as a minimum).
3.2.1 Assessment
Following detection/recognition of an incident/outbreak a member of IPCT or HPT will:
- Undertake an initial assessment, utilising the Healthcare Infection Incident Assessment Tool (HIIAT) - Appendix 14, gather epidemiological data and clinical assessment information on the patient's condition as per:
- NHS boards are required to report all HIIAT assessed Green, Amber and Red reports to ARHAI Scotland through the electronic outbreak reporting tool (ORT). See section 3.2.3.
- NHS boards should monitor the ongoing impact of the incident by escalating and de-escalating as appropriate, using the HIIAT assessment tool. The HIIAT assessment should remain Amber or Red whilst there is ongoing risk of exposure, identification of new cases.
3.2.2 Investigation, management and communication
The IPCT/HPT will establish an IMT if required.
- In the NHS hospital setting the ICD will usually chair the IMT and lead the investigation of healthcare incidents. Where there are implications for the wider community e.g., TB or measles, or rare events such as CJD or a Hepatitis B/HIV look back, or where there is an actual or potential conflict of interest with the hospital service, the CPHM may chair the IMT. A draft agenda for the IMT is available.
- The membership of the IMT will vary depending on the nature of the incident.
- A healthcare infection incident investigation will usually consist of the following elements: an epidemiological investigation, a microbiological investigation and a specific investigation to identify how cases were exposed to the infectious agent (environmental investigation)
- As part of the epidemiological investigation, a case definition(s) must be established by the IMT. A case definition should include the following: the people involved (for example, patients, staff), the symptoms/pathogen/infection (for example, with Group A Streptococci), the place (for example, care area(s) involved) and a limit of time (for example, between January and March year/date). The case definition(s) should be regularly reviewed and refined (if required) throughout the incident investigation as more information becomes available. A working hypothesis regarding the transmission route and source of the exposure must be formed based on initial investigation findings.
- A microbiological investigation into the nature and characteristics of the implicated hazard /infective agent must be conducted.
- Typing and whole genome sequencing can support outbreak and incident investigations. These services are available for some organisms and details of the services available should be discussed with your laboratory. Public Health Scotland continue to offer a SARS-CoV-2 whole genome sequencing service to support outbreak investigations and address important clinical and epidemiological questions.
- An environmental investigation must be conducted if the findings of the epidemiological investigation suggest a common exposure to a potential environmental source/environmental reservoir.
- Review of patient cases should consider any potential missed opportunities to isolate a patient, a delay in which may have resulted in onward transmission. Any learning should be widely communicated to all clinical staff in the board.
- An infection prevention and control assessment to review the existing IPC practices must be conducted, so that areas for immediate improvement can be identified.
- The IMT should receive and discuss all information gathered and epidemiological outputs for example an epidemiological (epi) curve, a timeline and a ward map to:
- determine whether additional case finding and control measures may be necessary
- confirm that all incident control measures are being applied effectively and are sufficient
- Control measures must be directed at the source of the exposure and/or at affected persons in order to prevent secondary/further exposure to the agent. Control measures must be initiated within 24 hours of receiving the initial report and should be implemented based on relevant guidance (for example pathogen specific) and investigation findings of the nature of the outbreak.
- A follow-up period may be defined after an infection incident/outbreak has ended to ensure its termination, including assessment of any ongoing control measures and would be determined by the PAG/IMT.
- Identify any change(s) in the system: staffing, procedures/processing, equipment, suppliers. A step-by-step review of procedure(s). An outbreak checklist is available.
- Identify and count all cases and/or persons exposed: This includes the total number of confirmed/probable/possible exposed cases. An incident/outbreak data collection tool is available.
If staff screening is being considered as part of the investigation DL (2020)1 must be followed.
- HAI deaths, which pose an acute and serious public health risk, must be reported to the Procurator Fiscal, refer to SGHD/CMO(2018)11.
- The IMT must ensure affected patients, and where appropriate their next of kin, have been informed of any actual or potential harm as a result of the HAI. Duty of Candour must be considered at each IMT.
- All significant adverse event reviews involving a category 1 adverse event (events that may have contributed to or resulted in permanent harm, for example unexpected death) should also be reported.
- If no new cases arise and any remaining cases are considered to no longer pose a risk, the IMT should agree on actions prior to resumption of normal service.
3.2.3 Communications
- Following the PAG/IMT, the NHS Board is required to communicate all HIIAT Green, Amber and Red assessments with ARHAI Scotland, by completing the electronic Outbreak Reporting Tool (ORT) within 24 hours of HIIAT assessment.
- Exported MS Excel files must be emailed to ARHAI Scotland for processing – the “Export Data File for ARHAI” button within the ORT only saves the extract from the ORT into the folder. Extracted data files should be emailed to the ARHAI Scotland ICT mailbox (NSS.ARHAIinfectioncontrol@nhs.scot).
- The Protocol for the Reporting of Healthcare Infection Incidents, Outbreaks and Data Exceedance in NHSScotland through the Outbreak Reporting Tool (ORT) is available in the resources section of the NIPCM.
- For incidents/outbreaks that are HIIAT assessed as Red, Amber or Green, frequency of updates are as follows:
- HIIAT Red – review, update and submit a daily update.
- HIIAT Amber– review, update and submit a twice weekly update.
- HIIAT Green – review, update and submit a weekly update.
- The Healthcare Infection Incident and Outbreak Reporting Template (HIIORT) form is for any HIIAT Red, Amber or Green assessed incident/outbreaks. Incidents assessed as Red, Amber or Green, where ARHAI support is requested, will be reviewed for onward communication to Scottish Government Healthcare Associated Infection Policy Unit.
- Respiratory incidents/outbreaks associated with key respiratory pathogens (COVID-19, influenza and respiratory syncytial virus (RSV)), should be completed within the Respiratory Short Form. However, where IPC measures do not align with the outbreak checklist and NIPCM, or where ARHAI support is requested a full HIIORT form must be completed. The Outbreak Checklist is available in the resources section of the NIPCM website.
- COVID-19 reporting should now align with reporting for other key respiratory pathogens (Influenza/RSV).
- Any adverse event related to equipment or medication must be reported as soon as possible (within one working day) to the Incident Reporting and Investigation Centre (IRIC) and the escalation/de-escalation flowchart followed.
Closure of incident/outbreak with lessons learned
- Once the incident is declared over, and in addition to reporting via the electronic outbreak reporting tool (ORT), the IMT/NHS board should decide on the most appropriate format for a report. This is to communicate any lessons learned using the Hot Debrief Tool. Completion of this and submission to ARHAI Scotland is not mandatory, but for the purposes of sharing lessons learned across Scotland.
The IMT Chair, in discussion with the IMT, should determine whether further reporting on the incident and the incident management is required i.e. SBAR Report and full IMT report template are available in the resources section of the NIPCM website.
Chapter 4 - Infection Control in the Built Environment and Decontamination
Introduction
Currently, chapter 4 exists as a repository for evidence reviews and tools relating to IPC in the built environment including delivery of appropriate decontamination within health and care settings and risk mitigation for water based pathogens.
Content going forward will be developed via the ARHAI Scotland Infection Control in the Built Environment and Decontamination (ICBED) programme informed by stakeholder engagement and requirements, learning from NHS Assurance programme and outbreaks and incidents.
Links to tools and guidance developed by ARHAI Scotland’s Clinical Assurance Programme will also be included within chapter 4.
This chapter is in the early stages of development.
Bed spacing
Guidance consistently recognises that bed spacing requirements contribute towards the control of HAIs. All NHS boards and care providers should aim to meet the minimum bed spacing requirements laid out in the guidance below and in keeping with the date of design and construction of the building. This takes account of ergonomics within the clinical environment and not just healthcare associated infection (HAI) risk. Some other health and care settings may choose to adopt this guidance e.g. hospice settings.
Adult in-patient facilities designed post 2010 should achieve 3.6m (width) x 3.7m (depth) dimensions of SHPN 04-01, HBN 00-03 and SHFN 30. Width of 3.6m is measured from bed centre to bed centre. Since 2014, HBN 00-03’s Figure 45 states a day treatment bay should achieve 2.45m width/centre-to-centre dimension.
Current NHS Scotland Guidance on bed spacing is listed below:
- Core guidance - General design for healthcare buildings (HBN 00-01)
- Core guidance - Clinical and clinical support spaces (HBN 00-03)
- Critical care units (HBN 04-02)
- HAI-SCRIBE Manual information for project teams (SHFN 30 Part A)
- HAI-SCRIBE Implementation strategy and assessment process (SHFN 30 Part B)
- HAI-SCRIBE question sets and checklists (SHFN 30 Part C)
- Adult in-patient facilities (SHPN 04-01)
- In-patient accommodation - supp 1 - Isolation facilities in acute settings (SHPN 4 sup 1)
Publications
Work undertaken and published to date has been cited here for ease of reference and use at a clinical level.
Many of these publications were produced prior to development of chapter 4 and were published outwith the existing manual methodology.
Updates to publications will be made where required as part of the ARHAI programme work plans.
ARHAI Scotland will work with SG directorates responsible for these areas in planning to establish planned implementation.
Decontamination
Probes
Equipment and environment cleaning
- NHSScotland Guidance for Decontamination and testing of Cardiac Heater Cooler Units (HCUs). v1.0 | National Services Scotland
Alternative approaches to decontamination
- Literature Review and Practice Recommendations: Existing and emerging technologies used for decontamination of the healthcare environment
Built environment
Water
- NHSScotland Guidance for the interpretation and clinical management of endoscopy rinse water
- Literature Review and Recommendations: Management of Dental Unit Waterlines
Clinical Assurance
ARHAI Scotland’s Clinical Assurance programme provides clinical and infection prevention and control (IPC) expertise to complement the work undertaken by the NHSScotland’s Assure (NHSSA) assurance service. More information about the programme and a list of tools and guidance developed is available.
Key Stage Assurance Reviews (KSAR) focus on ensuring infection prevention and control is a key consideration for healthcare construction projects. ARHAI Scotland have developed notes for NHS Board IPC Teams which aim to help navigate this process.
Below is an educational animation which focuses on clinical hand wash basins (CHWBs), their intended purpose, water associated infection risks, and what we all can do together to reduce this risk. The animation is supported by a poster for use beside CWHBs to locally promote good practice for health and care staff as well as the general public who may visit those settings.
Addendum for Infection Prevention and Control within Neonatal Settings (NNU)
The purpose of this addendum is to provide additional guidance to chapters 1,2 and 3 for NNUs.
4.1 Placement of neonates/assessment for infection risk
Undertake assessment for infection risk at the point of entry into the unit before placement of the neonate is decided. This assessment is the minimal microbiological testing required and any additional testing would be determined by the clinical presentation of the neonate. The potential for transmission of infection should be continuously reviewed throughout the stay/period and must be documented in the clinical notes.
Neonates who present as a cross infection risk include those who:
- have been transferred from another unit in Scotland with an ongoing incident/outbreak or
- were born outside Scotland
- have previously been positive with a Multidrug Resistant Organism (MDRO), or any alert organism or alert condition as found in Appendix 13.
From mothers who have:
- been hospitalised outside Scotland in the previous 12 months
- had no antenatal care
- been previously positive with a MDRO e.g. Meticillin Resistant Staphylococcus Aureus (MRSA) or Carbapenemase Producing Enterobacterales (CPE)
If a neonate is considered to be a cross infection risk then the clinical judgement of those involved in the management of the baby should assess the placement by prioritising the incubator/cot in a suitable area pending investigation i.e. place in a single room or cohort area/room with a wash hand basin.
Information/advice must be given to parents/carers of all neonates; particularly during outbreaks/incidents
4.2 Healthcare infection, incidents, outbreaks and data exceedance
In addition to the definitions in Chapter 3, in a neonatal unit investigation by IPCT is also required if:
- a single case of Pseudomonas aeruginosa is identified
- a single case of infection with an alert organism is identified
- two or more cases of colonisation with the same organism; linked in time and place are identified
Additionally, the local IPC team should consider the possibility of any onward transmission and potential for an incident/outbreak where there is:
- A single case of colonisation with an alert organism identified
Assigning a dedicated team to care for infected or colonised neonates may also be required. During outbreaks or incidents the ratio of staff to neonates may need to increase and it may be necessary to restrict admissions to the area. Prior to closing or restricting a neonatal unit, communication must be agreed across neonatal services and risk assessed.
Transfers to other units during incidents or outbreaks should be avoided, where possible; however this should take into consideration the clinical needs of neonates, and any practical or logistical issues for parents/carers.
4.3 Personal care of neonates
Due to the vulnerability of some neonates the use of tap water for personal care requires consideration and this is outlined in Guidance for neonatal units (NNUs) (levels 1, 2 & 3), adult and paediatric intensive care units (ICUs) in Scotland to minimise the risk of Pseudomonas aeruginosa infection from water. For example, an assessment should be made on the neonate’s condition and whether tap water can be used or if an alternative, such as sterile water, is considered more appropriate.
In addition incubators/cots should not be placed near any water source where spraying or splashing may occur.
Further information for neonatal IPC management of healthcare incidents and outbreaks can be found in the supporting literature review.
Neonatal resources
Quality improvement tools provide short practice points which when followed correctly can help reduce HAIs and improve patient safety.
These quality improvement tools are based on scientific literature reviews and practice recommendations from ARHAI Scotland.
Materials including posters are available for the following procedures/situations:
Care Home Infection Prevention and Control Manual (CH IPCM)
When an organisation uses products or adopts practices that differ from those stated in this Care Home Infection Prevention and Control Manual, that individual organisation is responsible for ensuring safe systems of work including the completion of risk assessments approved through local governance procedures.
Use of this manual online is advised as printed versions are uncontrolled.The ARHAI Scotland Transmission Based Precautions (TBPs) literature review is currently ongoing and so the information may be subject to change.
Last updated: 28 August 2023
What is the Care Home Infection Prevention and Control Manual (CH IPCM)?
The Care Home Infection Prevention and Control Manual (CH IPCM), referred to as ‘the manual’ throughout, was first published in 2021. It is evidence-based and is intended to be used by all those involved in care home provision in Scotland.
The manual is context specific and has been co-produced with national and local stakeholders. The content of the manual is completely aligned to the evidence based National Infection Prevention and Control Manual (NIPCM) which was first published in 2012, by the Chief Nursing Officer (CNO (2012)1).
The manual currently contains
- Chapter 1 – Standard Infection Control Precautions (SICPs)
- Chapter 2 – Transmission Based Precautions (TBPs)
The manual is a practice guide for use in care homes. When used, it can help reduce the risk of infections and ensure the safety of residents, as well as staff and visitors in the care home environment. It is the Scottish Government expectation that care home settings apply guidance contained within this manual to achieve the aims.
The manual aims to:
- make it easy for staff to apply effective infection prevention and control (IPC) precautions
- help reduce the risk of infection
- reduce variation, promote standardisation, and optimise IPC practices throughout care home settings
- improve the application of staff knowledge and skills in IPC
- help align practice, monitoring, quality improvement and scrutiny
The manual should be adopted for all IPC practices and procedures within care home settings.
Is the manual based on scientific literature?
The recommendations for practice made in the manual are fully aligned to the NIPCM and are based on real-time reviews of the current scientific literature (for example Medical Journals) and best practice. Any major changes identified in the scientific literature may lead to a change being made to the content, and so, it is recommended that the online version is always accessed and used locally.
What's in the appendices?
The appendices can be used as practical implementation of the manual and contain graphical representations (for example diagrams and charts) that can be used along with the contents of the manual.
Many of the appendices can be printed off as posters for local use throughout the care home.
Are there any other IPC materials that can be used?
There are links throughout the manual to additional resources and the resources page links to IPC campaign materials, education, training links and posters.
In addition you may find it useful to read the literature reviews and SBARs for the manual.
How can I find out what the scientific and medical words mean?
A glossary section has been provided.
Does the manual content work on mobile devices?
Yes, all content including appendices work on mobile devices for example laptops and smartphones.
Responsibilities for the CH IPCM
Responsibilities for content of the manual
ARHAI Scotland to ensure:
- that the content of this manual remains evidence based or where evidence is lacking, content is based on consensus of expert opinion
Stakeholders of ARHAI Scotland programme working groups to ensure:
- full participation in the working groups including full engagement with the consultation process outlined in the Terms of Reference associated with each working group
Responsibilities for the adoption and implementation of this manual
The manual should be used by:
- care home organisations
- care home staff including permanent, agency and where required external contractors
- health protection teams
- infection prevention and control teams
- professionals providing support
- individuals visiting the care home
Care home providers to ensure:
- the adoption and implementation of this manual in accordance with existing local governance processes
- that systems and resources are in place to facilitate implementation and compliance monitoring of IPC as specified in this manual in all care areas
- compliance monitoring includes all staff (permanent, agency and where required external contractors)
- there is an organisational culture which promotes incident reporting and focuses on improving systemic failures that encourage safe IPC working practices including near misses
- there is a nominated lead with responsibility for IPC within the care home
Care home managers to ensure that all staff:
- are aware of and have access to this manual
- have completed appropriate IPC training relevant to their roles and that this is centrally recorded. Training may include resources developed by your organisation, your local NHS board, Health and Social Care Partnership, NHS Education for Scotland (NES) or the Scottish Social Services Council (SSSC)
- have adequate support and resources available to enable them to implement, monitor and take corrective action to ensure full compliance with this manual
- implement a robust risk assessment including detailing any deviations from the manual and the local mitigation measures that were undertaken and post-approval documented via local governance procedures
- with health concerns (including pregnancy) or those who have had an occupational exposure relating to IPC are timeously referred to the relevant agency, for example general practitioner (GP or doctor), occupational health or if required accident and emergency
- have undergone the required health checks or clearance (including those undertaking exposure prone procedures (EPPs))
- include IPC as an objective in their personal development plans (or equivalent)
Care home staff providing care to:
- understand, adopt and implement the principles of IPC as set out in this manual
- maintain IPC competence, skills, and knowledge through completing appropriate training relevant to their role as directed by their line manager. IPC training, NHS Education for Scotland (NES) or the Scottish Social Services Council (SSSC)
- communicate the IPC practices to be taken to appropriate colleagues, residents, relatives and visitors without breaching confidentiality
- have up to date occupational immunisations/health checks/clearance requirements as appropriate
- report to line managers and document any gaps in IPC knowledge, resources, equipment and facilities or incidents that may result in transmission of infection including near misses for example sharps or PPE failures
- do not provide care while at risk of potentially transmitting infectious agents to others - if in any doubt they should consult with their line manager, occupational health department, local infection prevention and control team (IPCT) or local health protection team (HPT)
- contact the local HPT/IPCT if there is a suspected or actual HAI incident/outbreak
Local infection prevention and control teams (IPCTs) and health protection teams (HPTs) to:
- engage with care home staff to develop systems and processes that lead to sustainable and reliable improvements in relation to the application of IPC practice
- provide expert advice on the application of IPC and provide support when requested to develop individual or organisational risk assessments where deviations from the manual are necessary
- have epidemiological or surveillance systems capable of distinguishing resident case or cases requiring investigations and control
- provide local support and advice (when necessary and/or requested) and complete documentation when an incident/outbreak or data exceedance is reported
Chain of infection
In order for infection to occur several things have to happen. This is often referred to as the chain of infection. The six links in the chain are:
- infectious agent or the microorganism which can cause disease
- reservoir or source of infection where the microorganism can live and thrive. This may be a person, an animal, any object in the general environment, food or water
- portal of exit from the reservoir. This describes the way the microorganism leaves the reservoir. For example, in the case of a person with flu, this would include coughing and sneezing. In the case of someone with gastroenteritis microorganisms would be transmitted in the faeces or vomit
- mode of transmission. This describes how microorganisms are transmitted from one person or place to another. This could be via someone’s hands, on an object, through the air or bodily fluid contact
- portal of entry. This is how the infection enters another individual. This could be landing on a mucous membrane, being breathed in, entering via a wound, or a tube such as a catheter.
- susceptible host. This describes the person who is vulnerable to infection.
Infection can be prevented by breaking the chain of infection.
The chain of infection diagram illustrates and gives examples of actions that can be taken to break it. The overall aim of Standard Infection Control Precautions (SICPs), is to break the chain of infection.
Select image for full size version.
![]() Use the NES SIPCEP Breaking the Chain of Infection module to learn about breaking the chain of infection in care homes.
Use the NES SIPCEP Breaking the Chain of Infection module to learn about breaking the chain of infection in care homes.
Reducing risk
The hierarchy of controls (HoC) is a system used to help prevent the transmission of infection. It details the most to least effective controls. You will note that PPE is the last level of control in the hierarchy, used when all other controls have not reduced the risks sufficiently. To be effective, PPE must be used correctly which means putting it on and removing it correctly and safely.
![]() See the Health and Safety Executive’s (HSE) toolkit on management of risk when planning work: the right priorities for additional information.
See the Health and Safety Executive’s (HSE) toolkit on management of risk when planning work: the right priorities for additional information.
The HoC principles can be broadly interpreted for care home settings and include:
- reducing hazards in the care home
- changing practice in the care home
- making the care home as safe as possible
- changing how we organise and work in the care home
- use of PPE
Examples of HoC principles
Here are some examples of how to apply the HoC principles in care home settings. These examples do not cover every situation where you might need to use HoC principles.
Reducing hazards in the care home
Measures such as vaccination, testing and isolation help to reduce the risk of infection. Not coming to work when ill, isolating while infectious and recognising and reporting infections promptly, all help to prevent infections spreading.
Changing practice in the care home
When faced with a particular risk, such as an outbreak, we may need to change what we do. This might include reducing communal activities, considering limiting visiting for a short period of time, or cleaning the care home environment more frequently. The local IPCT and/or HPT should always be contacted for advice and support in outbreak situations.
Making the care home as safe as possible
It is very unlikely that we will be able to change where we work but the care home setting should be made as safe as possible. You can reduce opportunities for pathogens to survive in the care home, ensuring fixtures and fittings are in good repair and can be easily cleaned and following water safety guidelines. Ventilation is also an effective measure to reduce the risk of some respiratory infections, by diluting and dispersing the pathogens which cause them. Consider opening windows and vents more than usual, even opening a small amount can be beneficial. Opening windows and doors may present security and safety issues and so a local risk assessment should always be undertaken.
Changing how we organise and work in the care home
Changing the way, we organise and work in the care home can also help reduce risk. This might include reducing the number of people in a space at any one time and minimising the movement of staff between different settings as well as using administrative controls. Administrative controls include local risk assessments, staff training, IPC audits, and providing clear signage and instructions throughout the care home.
Chapter 1: Standard Infection Control Precautions (SICPs)
The basic IPC measures that should be used in your care home are called Standard Infection Control Precautions (SICPs).
SICPs are used to reduce the risk of transmission of infectious agents from known and unknown sources of infection.
These should be used by all staff, in all care settings, at all times, for all residents whether infection is known to be present or not to ensure the safety of residents, staff and visitors in the care home.
SICPs should be part of everyday practice and applied consistently by everyone in the care home.
It is essential that optimal IPC measures are applied continuously as residents living in care homes are more vulnerable, therefore increasing their risk of acquiring infections which may then be serious and potentially life threatening. By applying optimum IPC precautions you will provide a safe environment and effective care.
There are 10 Standard Infection Control Precautions (SICPs)
- resident placement/assessment for infection risk
- hand hygiene
- respiratory and cough hygiene
- personal protective equipment
- safe management of care equipment
- safe management of care environment
- safe management of linen
- safe management of blood and body fluid spillage
- safe disposal of waste
- occupational safety: prevention and exposure management (including sharps)
1. Resident placement/assessment for infection risk
For residents being discharged from hospital to a care home/hospice the Public Health Scotland COVID-19 information and guidance for social, community and residential care settings should be followed.
Before a resident is admitted to the care home it is important to risk assess for infection as part of resident’s care plan, an IPC admission assessment should be undertaken by staff.
If you suspect or are aware that a resident has an infection, then details should be confirmed for the correct IPC precautions to be put in place for the safety of the resident and others.
Obtaining infection details may include appropriate clinical samples and/or screening to establish the causative organism which may be on advice from your local GP, IPCT or HPT.
Residents who may present a cross-infection risk include those with:
- diarrhoea
- vomiting, being sick
- unexplained rash
- fever or temperature of 37.8 C or higher
- respiratory symptoms such as coughing and sneezing
- known to have been previously positive with a Multi-drug Resistant Organisms (MDRO), for example Meticillin Resistant Staphylococcus aureus (MRSA), Carbapenemase Producing Enterobacterales (CPE)
Further information regarding general respiratory screening questions can be found within the resources section of the NIPCM.
Note: If a resident requires isolation because of infection or in an outbreak situation, this should be individually risk assessed to ensure the safety and health and wellbeing needs of the resident. Isolation periods must be monitored on daily basis and be for the minimum period specified.
Resources
![]() Appendix 11 of the NIPCM gives you further information on the precautions required for different infections.
Appendix 11 of the NIPCM gives you further information on the precautions required for different infections.
 Read the placement literature review to understand the evidence base for resident placement.
Read the placement literature review to understand the evidence base for resident placement.
2. Hand hygiene
Please note that the term ‘alcohol-based hand rub (ABHR)’ has now been updated to ‘hand rub’. A hand rub (alcohol or non-alcohol based) can be used if it meets the required standards. Please see further information in the hand hygiene products literature review.
 The most important thing you can do to prevent the spread of infection in a care home is to keep your hands clean. This is called hand hygiene.
The most important thing you can do to prevent the spread of infection in a care home is to keep your hands clean. This is called hand hygiene.
Hand washing sinks should only be used for hand hygiene and should not be used for the disposal of other liquids (See Appendix 3 of Pseudomonas Guidance for further information).
Before performing hand hygiene:
- expose forearms (known as bare below the elbows)
- remove all hand/wrist jewellery including any embedded jewellery (a single, plain metal finger ring or ring dosimeter (radiation ring) is permitted but should be removed (or manipulated) during hand hygiene). Bracelets or bangles such as the Kara which are worn for religious reasons should be able to be pushed higher up the arm and secured in place to enable effective hand hygiene which includes the wrists
- ensure fingernails are clean, short and that artificial nails or nail products are not worn
- cover all cuts or abrasions with a waterproof dressing
Hand washing should be extended to the forearms if there has been exposure of forearms to blood and/or body fluids.
To perform hand hygiene:
- hand rub should be available for staff as near to point of resident care as possible. Where this is not practical, personal hand rub dispensers should be used
- application of sufficient volume of hand rub to cover all surfaces of the hands is important to ensure effective hand hygiene
- manufacturer’s instructions should be followed for the volume of hand rub required to provide adequate coverage for the hands. In the absence of manufacturer’s instructions, volumes of approximately 3ml are recommended to ensure full coverage
- wall mounted or personal hand rub dispensers (cartridges/bottles) should not be refilled and should be replaced when empty or if outwith manufacturer expiry date
The World Health Organization’s ‘4 moments for hand hygiene’ should be used to highlight the key indications for hand hygiene:
- before touching a resident
- before clean/aseptic procedures. If hand rub cannot be used, then antimicrobial liquid soap should be used
- after body fluid exposure risk
- after touching a resident
Some additional examples of hand hygiene moments include, but are not limited to:
- after touching a resident’s immediate surroundings
- before handling medication
- before preparing food
- before donning (putting on) and after doffing (taking off) PPE
- after visiting the toilet
- before putting on and after removing PPE
- between carrying out different care activities on the same resident
- after cleaning and disinfection procedures
- after handling used linen
- after handling waste
It is important that residents are routinely encouraged to perform hand hygiene and given assistance if required.

The four moments for hand hygiene poster can be used in your care home to show staff when hand hygiene should be done and the reasons why.
Select image for full size version.

Hands should be washed with liquid soap and water if/when:
- they are visibly soiled or dirty
- they are potentially contaminated with blood, other body fluids or excretions
- caring for a resident with vomiting or diarrhoeal illness
- caring for a resident with a suspected or known gastro-intestinal infection such as norovirus or a spore forming organism such as Clostridioides difficile
Note:
Hands should be washed with warm/tepid water to mitigate the risk of dermatitis associated with repeated exposures to hot water and to maximise hand washing compliance. Compliance may be compromised where water is too hot or too cold.
Hands should be dried thoroughly following hand washing using a soft, absorbent, disposable paper towel from a dispenser which is located close to the sink but beyond the risk of splash contamination.
The use of antimicrobial hand wipes is only permitted where there is no access to running water. Staff should perform hand hygiene using ABHR immediately after using the hand wipes and perform hand hygiene with soap and water at the first available opportunity.
In all other circumstances use hand rub for routine hand hygiene.
Skin care
- Hand rubs should contain emollients in their formulation.
- Pat hands dry after hand washing using disposable paper towels. Avoid rubbing which may lead to skin irritation/damage.
- Use an emollient hand cream during breaks and when off duty. These should be applied all over the hands including between the fingers and the back of the hands.
- Staff with skin problems should seek advice from the local occupational health department if available or their GP.
- Barrier creams should not be used in the workplace.
Do not use refillable containers or communal tubs of hand cream in the care home setting.
Resources

Read the hand hygiene literature reviews to find out more about the evidence base for hand hygiene.
 To make sure you clean your hands properly with soap and water you should follow the steps in the poster ‘How to hand wash step by step images’. This poster can be printed off and displayed throughout the care home to ensure that all staff and visitors are aware of and practice this hand hygiene method when required in the care home.
To make sure you clean your hands properly with soap and water you should follow the steps in the poster ‘How to hand wash step by step images’. This poster can be printed off and displayed throughout the care home to ensure that all staff and visitors are aware of and practice this hand hygiene method when required in the care home.
Select image for full size version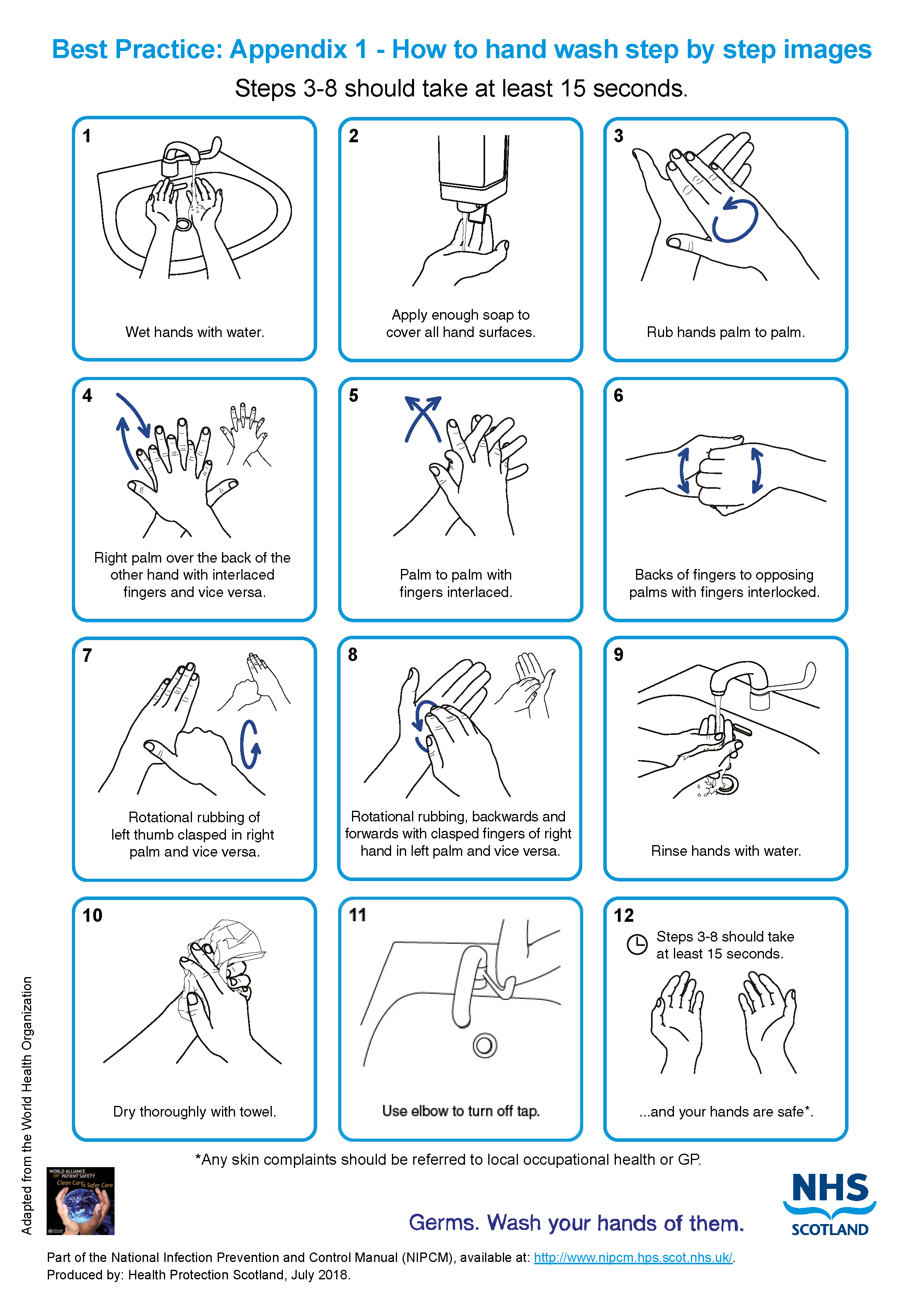
 To make sure you clean your hands properly with hand rub you should follow the steps in the poster ‘How to hand rub step by step images’. This poster can be printed off and displayed throughout the care home to ensure that all staff and visitors are aware of and practice this hand hygiene method when required in the care home.
To make sure you clean your hands properly with hand rub you should follow the steps in the poster ‘How to hand rub step by step images’. This poster can be printed off and displayed throughout the care home to ensure that all staff and visitors are aware of and practice this hand hygiene method when required in the care home.
Select image for full size version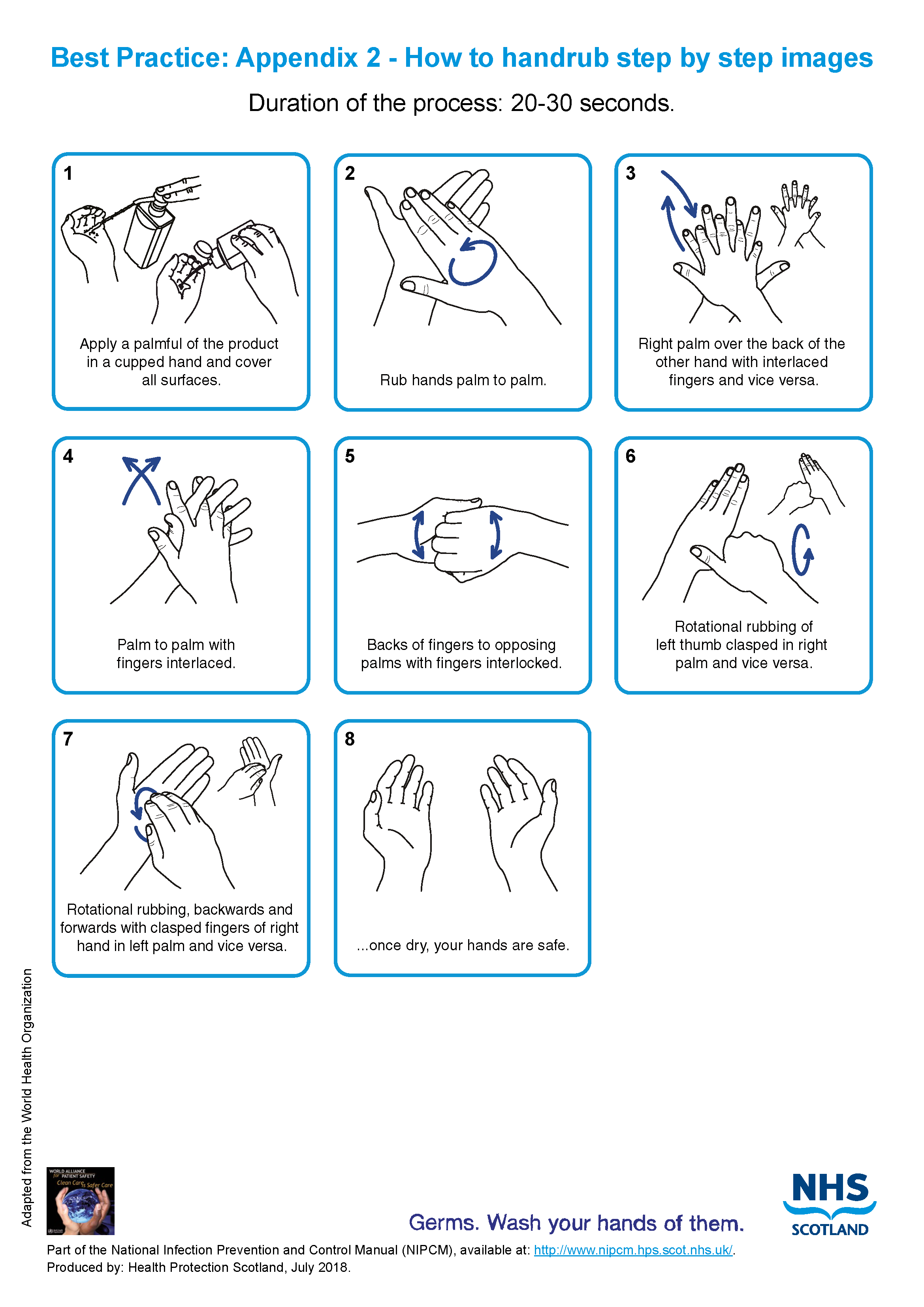
3. Respiratory and cough hygiene
Infections can spread by coughing and sneezing, therefore it is very important that respiratory and cough hygiene is used by everyone including staff, residents and visitors.
Any resident displaying symptoms of respiratory illness should be encouraged to wear a surgical (for instance TYPE IIR FRSM) face mask where it is clinically safe and can be tolerated by the wearer, especially in communal areas.
What you need for respiratory and cough hygiene• disposable tissues• waste bin and waste bags• hand hygiene products
If a resident has a cough, cold or other respiratory symptoms then they should be supported and encouraged to:
- cover their nose and mouth with a disposable tissue when sneezing, coughing, wiping and/or blowing the nose. If a disposable tissue is not available encourage the use of elbow/sleeve to cover the nose and mouth when coughing or sneezing
- put used tissues and face masks into a waste bin immediately after use
- wash their hands with soap and water after coughing, sneezing, using tissues, or after contact with respiratory secretions or objects contaminated by these secretions
- keep contaminated hands away from the eyes nose and mouth
Staff should:
- promote respiratory and cough hygiene and help residents who need assistance
- ensure that residents are provided with the necessary products for respiratory and cough hygiene including tissues, waste bag and hand hygiene products and make sure that products are in close vicinity for the resident to access
- use hand wipes followed by hand rub if there is no running water available or if hand hygiene facilities are out of reach then wash hands at the first available opportunity.
 Read the respiratory and cough hygiene literature review to find out the evidence for respiratory and cough hygiene practice.
Read the respiratory and cough hygiene literature review to find out the evidence for respiratory and cough hygiene practice.
4. Personal Protective Equipment (PPE)
PPE products you might need in the care home:• gloves• aprons• masks• eye protection
Deciding which PPE to use
Before doing any procedure or task staff should risk assess any likely exposure to blood and/or body fluids and ensure PPE is worn that provides adequate protection against the risks associated with the procedure or task being undertaken.
All PPE should be:
- located close to the point of use
- stored in a clean and dry area to prevent contamination until needed for use
- within expiry dates
- single-use only items unless specified by the manufacturer
- changed immediately after individual use and/or following completion of a procedure or task
- disposed of after use into the correct waste stream, this means healthcare waste or domestic waste
Reusable PPE items, for example non-disposable goggles, face shields and visors, should have a decontamination schedule with responsibility assigned.

Read further information on best practice for PPE in Appendix 16.
Donning (putting on) personal protective equipment (PPE)
The order for putting on PPE is:
- apron or gown
- surgical mask
- eye protection (where required)
- gloves
Doffing (taking off) personal protective equipment (PPE)
It is important that PPE is removed in the correct order.
The order for taking off PPE is:
- gloves
- apron or gown
- eye protection (if worn)
- surgical mask
Note:
Always carry out hand hygiene immediately after taking off PPE.
All PPE should be removed before leaving the area and disposed of as healthcare waste
Resources
A video demonstrating the order for donning and doffing PPE is available.
The correct order for donning, doffing and disposal of PPE for healthcare workers from NHS National Services Scotland on Vimeo.
 A poster showing the order for putting on and removing PPE is available to print.
A poster showing the order for putting on and removing PPE is available to print.
Select image for full size version
Gloves
Gloves should be:
- worn when it is likely or anticipated that you will be exposed to blood, body fluids (including but not limited to secretions and/or excretions), non-intact skin, mucous membranes, lesions and/or vesicles, hazardous drugs, and chemicals for example cleaning agents
- single-use and should be donned (put on) immediately prior to exposure risk and should be doffed (taken off) immediately after each use or upon completion of a task
- appropriate for use, fit for purpose and well-fitting. The glove selection chart can help you select the correct gloves
- changed if damaged or a perforation or puncture is suspected
Note:
Using gloves reduces the risk of contamination but does not remove all risk.
Gloves should not be used instead of carrying out hand hygiene.
Gloves should not be worn inappropriately in situations such as to go between residents, move around a care area or whilst at workstations (on the telephone or computer).
Gloves should never be decontaminated or cleaned with hand rub or by washing with cleaning products.
![]() Use the glove selection chart to support you to select the correct glove type.
Use the glove selection chart to support you to select the correct glove type.
Select image for full size version
Aprons and gowns
Aprons should be:
- worn by care staff when there is a risk of clothing being contaminated with blood or other body fluids
- worn during direct care, for example oral hygiene, bed-making or when undertaking the decontamination of equipment
- changed between residents and following completion of a procedure or task
The choice of apron or gown is based on an individual risk assessment and anticipated level of blood/body fluid exposure. Routine sessional use of gowns/aprons is not permitted.
Eye/face protection
Eye/face protection (including full face visors) should:
- be worn if blood and/or body fluid contamination to the eyes/face is expected/likely and always during aerosol generating procedures (AGPs)
Note:
Eye/face protection (including visors) should not be touched when worn.
Facial accessories such as piercings or false eyelashes should not be worn when using eye/face protection.
Regular glasses or safety glasses are not considered eye protection.
Fluid Resistant Type IIR surgical face masks (FRSM)
Fluid Resistant Type IIR surgical face masks should be:
- worn if splashing or spraying of blood, body fluids, secretions or excretions onto the respiratory mucosa (nose and mouth) is expected/likely. (As part of SICPs a full-face visor may be used as an alternative to fluid resistant Type IIR surgical face masks to protect against splash or spray)
- well-fitting, fully covering the mouth and nose and fit for purpose. Manufacturer’s instructions should be followed to ensure effective fit/protection
- removed or changed:
- at the end of a procedure/task
- if the mask is damaged or there is a build up from moisture after prolonged use or from gross contamination with blood or body fluids
- following specific manufacturers’ instructions
If you are using droplet precautions, you should always wear a Type IIR surgical face mask as well as the full-face visor (droplet precautions will be discussed further in Chapter 2 Transmission Based Precautions).
Transparent face masks
Transparent face masks may be used to aid communication with residents where required.
Transparent face masks should:
- meet the specification standards of the Transparent face mask technical specification
and
- have been approved for use within health and social care settings
- only be worn in areas where Fluid Resistant Type IIR surgical face masks are used as personal protective equipment
Resources
 Read the aerosol generating procedures literature review and surgical face masks literature review for further information regarding the evidence base.
Read the aerosol generating procedures literature review and surgical face masks literature review for further information regarding the evidence base.
See appendix 11 for further information.
PPE for visitors
At times, PPE may be offered to visitors to protect them from acquiring a transmissible infection. If a visitor declines to wear PPE when it is offered then this should be respected, and the visitor should not be refused entry to the care home. PPE use by visitors cannot be enforced and there is no expectation that staff monitor PPE use amongst visitors. Below is the PPE which should be worn where it is appropriate to do so and when the visitor chooses to do so.
Visitors do not routinely require PPE unless they are providing direct care to residents they are visiting.
Table 1 is a guide to PPE for use by visitors if delivering direct care.
Table 1: PPE for use by visitors
|
IPC Precaution |
Gloves |
Apron/Gown |
Face covering/mask |
Eye/face protection |
|
Standard Infection Control Precautions (SICPs) |
Not required*1 |
Not required*2 |
Where splash/spray to nose/mouth is anticipated during direct care |
Not required*3 |
|
Transmission Based Precautions (TBPs) |
Not required*1 |
Not required*2 |
If within 2 metres of resident with suspected or known respiratory infection |
If within 2 metres of resident with suspected or known respiratory infection |
*1 Unless providing direct care which may expose the visitor to blood and/or body fluids, for instance toileting.
*2 Unless providing care resulting in direct contact with the resident, their environment or blood and/or body fluid exposure, for instance toileting, bed bath.
*3 Unless providing direct care and splashing/spraying is anticipated.
 Read the PPE literature reviews to find out more information about the evidence base for PPE use.
Read the PPE literature reviews to find out more information about the evidence base for PPE use.
5. Safe management of care equipment
Care equipment is easily contaminated with blood, other body fluids, secretions, excretions and infectious agents and this can spread infection.
Important words and what they meanRoutine cleaning is regular cleaning which is carried out on a scheduled basis, not on an unplanned basis and not in response to an outbreak. For routine cleaning general purpose detergent and water solution or detergent impregnated wipes are sufficient.Cleaning is the removal of any dirt by use of an appropriate cleaning agent such as detergent.Decontamination is removing, or killing pathogens on an item or surface to make it safe for handling, re-use or disposal, by cleaning, disinfection and/or sterilisation.Disinfectant is a chemical used to reduce the number of infectious agents from an object or surface to a level that means they are not harmful to health.Detergent is a chemical cleansing agent that can dissolve oils and remove dirt.
If the resident has a known infection or the equipment is contaminated with blood or body fluids, then a disinfection agent needs to be used.
Note:
Do not use household bleach as the required dilution cannot be guaranteed.
Do not refill spray containers for cleaning products as there is a risk of contamination.
What you need for safe management of care equipment
- Cleaning/disinfectant products:
- general purpose detergent and water solution/detergent impregnated wipes
or
-
- combined detergent/disinfectant solution at a dilution of 1,000 parts per million available chlorine (ppm available chlorine (av.cl.)
or
-
- a general purpose neutral detergent in a solution of warm water followed by disinfection solution of 1,000ppm av.cl.
- Paper towels/disposable cloths.
Types of equipment
There are three different types of care equipment that you will use in your care home and it is important that you know how to deal with each type.
You should follow manufacturers guidance for all equipment and products you use including those used for cleaning and decontamination.
Before using any sterile equipment, you should check that:
- the packaging is intact
- there are no obvious signs of packaging contamination
- the expiry date remains valid
1. Single-use - equipment which is used once on a single resident and then discarded.
Single-use equipment must never be reused even on the same resident. The packaging carries the symbol.

Note:
 Needles and syringes are single-use devices. They should never be used for more than one resident or reused to draw up additional medication.
Needles and syringes are single-use devices. They should never be used for more than one resident or reused to draw up additional medication.
Never give medications from a single-dose vial or intravenous (IV) bag to multiple residents.
2. Single individual use – equipment which can be reused by same resident for example a sling and decontaminated following use as per manufacturers instructions.
3. Reusable non-invasive equipment (often referred to as ‘communal equipment’) – equipment which can be reused on more than one resident following decontamination between each use for example commode, moving and handling equipment or bath hoist.
Cleaning or decontaminating reusable non-invasive equipment
Residents should be given their own reusable (communal) non-invasive equipment where possible.
Reusable equipment should be checked frequently for cleanliness and signs of integrity. This will include mattresses and pillows which should be clean, have a waterproof covering which is in a good state of repair.
Pillows used on resident’s beds may not require a waterproof cover if they are single resident use and are subject to regular checks/laundering. Resident pillows may require labelling where appropriate.
Reusable equipment should be cleaned or decontaminated:
- between individual use
- after blood and/or body fluid contamination
- as part of the regular scheduled cleaning schedules/process
- before inspection, servicing or repair
Staff should:
- follow the local cleaning protocol/schedule which should include responsibility for, frequency of and method of decontamination required
- use a general purpose detergent and water solution/detergent impregnated wipes
or
a combined detergent/disinfectant solution at a dilution of 1,000 parts per million available chlorine (ppm available chlorine (av.cl.)
or
a general purpose neutral detergent in a solution of warm water followed by disinfection solution of 1,000ppm av.cl;
- make up cleaning/disinfection solution following manufacturers guidance
- follow the manufacturer’s contact time for the cleaning/disinfection solution
- rinse and dry reusable equipment then store it clean and dry
Note: When an organisation use products or adopts practices that differ from those stated in this manual, that individual organisation is responsible for ensuring safe systems of work including the completion of risk assessments approved through local governance procedures.
Resources
 Read the management of care equipment literature review to find out more about why we do things this way for care equipment.
Read the management of care equipment literature review to find out more about why we do things this way for care equipment.
 The decontamination of non-invasive care equipment poster can help staff decide how to clean equipment.
The decontamination of non-invasive care equipment poster can help staff decide how to clean equipment.
Select image for full size version
6 - Safe management of the care environment

 There are many areas in care homes that become easily contaminated with microorganisms (germs) for example door handles, toilets, waste bins, surfaces.
There are many areas in care homes that become easily contaminated with microorganisms (germs) for example door handles, toilets, waste bins, surfaces.
Furniture and floorings in a poor state of repair can have microorganisms (germs) in hidden cracks or crevices.
To reduce the spread of infection, the environment should be kept clean and dry and where possible clear from clutter and equipment.
Non-essential items should be stored and displayed in such a way as to aid effective cleaning
Keeping a high standard of environmental cleanliness is important in the care home as the residents are often elderly and vulnerable to infections.
The care home environment should be:
- visibly clean, free from non-essential items and equipment to help make cleaning effective
- well maintained and in a good state of repair
- routinely cleaned in accordance with the specified cleaning schedules:
- a fresh solution of general purpose neutral detergent in warm water is recommended for routine cleaning. This should be changed when dirty or at 15 minutes’ intervals or when changing tasks
- routine disinfection of the environment is not recommended. However, 1,000 parts per million available chlorine (ppm available chlorine (av.cl.) should be used routinely on sanitary fittings
Staff should:
- report any issues with the environment cleanliness or maintenance to the person in charge to ensure that the care environment is safe. The person in charge should then act on problems reported to them
- be aware of the environmental cleaning schedules and clear on their specific responsibilities
Cleaning schedules should include:
- staff responsibilities
- cleaning frequencies
- cleaning methods
Managing cleaning services
Cleaning services should be managed in a systematic way, and staff responsible for cleaning should be appropriately trained to carry out the tasks they are responsible for.
The care home manager is responsible for managing the cleaning service which has a number of essential elements outlined in the cleaning services diagram.
Select the Care Homes Cleaning Specification for full size version of cleaning services diagram.
Select the diagram for full size version
Cleaning Services
An effective service will include all of the elements above.
Care Homes Cleaning Specification
The Care Homes Cleaning Specification provides a guide to planning cleaning services. It has tools to help with the planning and recording of cleaning activities and with the management activities marked with a * in the diagram above. These include:
- a structure to identify all spaces within a care home and plan appropriate cleaning tasks and frequencies
- a set of weekly and monthly cleaning templates to be assigned to each space within a care home. These can be used to develop a schedule and to provide a method for recording all cleaning activity
Table 2 provides an example of a cleaning schedule and record. These tools are examples and designed to support local practice, however care homes can use their own tools if preferred. If a local tool is used, it should reflect the standards set out in the Care Homes Cleaning Specification.
Table 2: Example cleaning schedule residents room
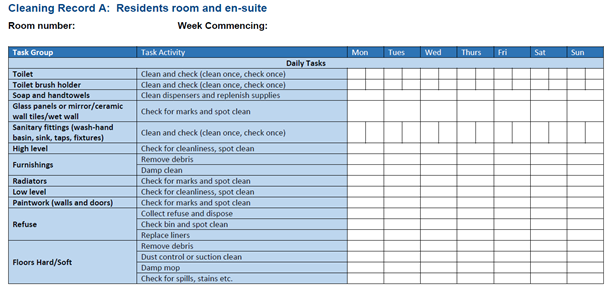
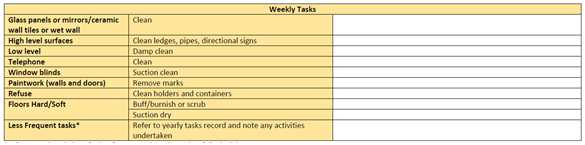
- Standard operating procedures (SOPs) for all cleaning tasks. Each SOP outlines the correct equipment, safety considerations, method, and outcomes required for each task. Table 3 shows the important steps that must be taken during the cleaning of floors.
Table 3: Example cleaning SOP: Floors
- A process for checking the cleanliness of the care environment, to ensure standards are being maintained and to identify areas for improvement.
The tools within the Cleaning Specification should be used by the care home manager in the planning, training of staff, delivery, and checking of standards of the cleaning services they provide.
Manufacturer’s instructions and recommended contact times should be adhered to.
Decontamination of soft furnishings
Decontamination of soft furnishings may require to be discussed with the local HPT/ICT. If the soft furnishing is heavily contaminated with blood or body fluids, it may have to be discarded. If it is safe to clean with standard detergent and disinfectant alone then follow appropriate procedure.
If the item cannot withstand chlorine releasing agents staff are advised to consult the manufacturer’s instructions for a suitable alternative to use following or combined with detergent cleaning.
Note: When an organisation adopts decontamination processes not recommended in the CH IPCM the care organisation is responsible for governance of and completion of local risk assessment(s) to ensure safe systems of work.
 Read the routine cleaning of the care environment literature review to find out more about why we do things this way for the care environment.
Read the routine cleaning of the care environment literature review to find out more about why we do things this way for the care environment.
7 - Safe management of linen
Examples of linen you may have in the care home includes:
- bed linen (bed sheets, duvet, duvet covers, pillowcases)
- blankets
- curtains
- hoist slings
- towels
- resident clothing
There are three categories of linen:
Clean – Linen washed and ready for use
Used – All used linen in the care setting not contaminated by blood or body fluids
Infectious – All linen used by a person known or suspected to be infectious and/or linen that is contaminated with blood or body fluids for example faeces
Used or infectious linen may also be categorised as heat-labile: usually personal clothing where the clothing may be damaged (shrinking/stretching) by washing at a higher than recommended temperature than the label advises and therefore, cannot be subject to thermal disinfection. If such linen needs to be washed at a higher temperature for example if soiled or resident has a known infection they or their relatives need to be advised that the clothing may be damaged.
All clean, used and infectious linen should be handled with care and attention paid to the potential spread of infection. Appropriate temperatures for processing all used and infectious linen should be adhered to achieve thermal disinfection.
Clean linen
- Should be stored in a clean, allocated area. This should be an enclosed cupboard but a trolley could be used as long as it is completely covered with a waterproof covering that is able to withstand cleaning.
Used linen
Staff should:
- put on disposable gloves and apron prior to handling used linen
- make sure that a laundry trolley or container is available as close as possible to the point of use for immediate linen deposit
Staff should not:
- rinse, shake or sort linen on removal from beds or trolleys
- place used linen on the floor or any other surfaces for example on a locker or tabletop
- re-handle used linen once bagged
- overfill laundry receptacles or trolleys
- place inappropriate items in the laundry receptacle for example used equipment/needles.
Infectious linen
Staff should:
- wear disposable gloves and apron before handling infectious linen
- put infectious linen directly into a water soluble laundry bag and secure before putting into a clear plastic bag and placing into a laundry receptacle/trolley
If using external laundry services both used and infectious linen bags/receptacles should follow local procedure and arrangements. Store all used/infectious linen in a designated, safe, lockable area whilst awaiting uplift.
All linen that is deemed unfit for re-use, for example torn or heavily contaminated, should be categorised at the point of use and disposed of in the appropriate local healthcare waste stream.
Washing residents personal linen
Appendix 1 National Guidance for Safe Management of Linen in NHSScotland Health and Care Environments - For laundry services/distribution contains information that is particularly relevant and may be useful for residential care settings where domestic-type (household) washing machines may be in place for laundering resident’s personal items and clothing.
Domestic-type washing machines are not typically programmed with the temperature settings required for thermal disinfection, therefore domestic-type machines may only be used for laundering personal items of clothing belonging to residents, such as those that are heat-labile.
Other types of used linen such as sheets should be reprocessed using a machine that is capable of a validated temperature disinfection stage.
If using a domestic type washing machine to launder resident’s personal items:
- wash items using the highest temperature you can and following the washing instructions
- use your normal washing powder or detergent and follow the instructions on the correct amount to use
- tumble-dry (if possible) following the washing instructions
- iron according to washing instructions. If possible, use a hot steam iron.
It is considered best practise to launder a resident’s personal items separately, that means not to mix items from multiple persons within a single load.
If visitors wish to take their relatives clothes home to be laundered, place laundry in an appropriate bag and provide them with a washing clothes at home leaflet.
If the residents clothing is very soiled or infectious, staff may recommend that the clothing is washed in the care home’s laundry service if available, otherwise, the item should be disposed of in the appropriate healthcare waste stream following discussion with the resident or their relative(s).
 Read the safe management of linen literature review to find out more about why we do things this way when dealing with linen.
Read the safe management of linen literature review to find out more about why we do things this way when dealing with linen.
8 - Blood and body fluid spillages
Spillages of blood and other body fluids may transmit blood borne viruses.
Important words and what they meanA blood borne virus is a virus carried or transmitted by blood, for example Hepatitis B, Hepatitis C and HIV.Body fluids are fluids produced by the body such as urine, faeces, vomit or diarrhoea. These body fluids may also contain blood.
Blood and body fluid spillages must be decontaminated:
- immediately by staff trained to undertake this safely
- using body fluid spill kits/equipment available
Responsibilities for the decontamination of blood and body fluid spillages should be clear within each area/care setting.
Resources
 Read the management of blood and body fluid spillages literature review to find out more about why we do things this way for blood and body fluid spillages.
Read the management of blood and body fluid spillages literature review to find out more about why we do things this way for blood and body fluid spillages.
 Use the poster management of blood and body fluids to help you when you clean up blood and body fluid spillages.
Use the poster management of blood and body fluids to help you when you clean up blood and body fluid spillages.
Select the image for full size
9 - Safe disposal of waste (including sharps)
Different types of waste will be produced within care homes.
Some waste may be disposed of through the domestic waste route but other types of waste needs special handling and disposal for example sharps and waste from people who have or may have an infection.
Waste bags in care settings should be colour coded to denote the various categories of waste.
Local procedures and policies on waste disposal should be followed.
Segregation (separating) of waste
- Healthcare (including clinical) waste is produced as a direct result of healthcare activities for example soiled dressings, sharps
- Special (hazardous) waste arises from the delivery of healthcare in both clinical and non-clinical settings. Special waste includes a range of controlled wastes, defined by legislation, which contain dangerous or hazardous substances for example chemicals and pharmaceuticals
- Domestic waste – must be segregated at source into:
- Dry materials that can be recycled (glass, paper and plastics, metals, cardboard)
- Residual waste (any other domestic waste that cannot be recycled)
Care home waste disposal may differ from categories described and guidance from local contractors may apply.
Safe management of waste
Care home managers and staff should ensure:
- all waste is correctly segregated according to local regulations
- correct colour coded bags are being used according to local regulations
- there is a dedicated area for storage of clinical waste that is not accessible to residents or the public
- waste is stored in a designated, safe, lockable area whilst awaiting uplift. Uplift schedules should be acceptable to the care area and there should be no build-up of waste receptacles
- there is a schedule for emptying domestic waste bins at the end of the day and during the day if needed
All staff should:
- follow local schedules for emptying domestic waste bins
- always use appropriate personal protective equipment (PPE)
- dispose of waste immediately as close as possible to where it was produced
- dispose of clinical waste into the correct UN 3291 approved waste bin or sharps container
- ensure that waste bins are never overfilled. Once the waste bin is three quarters full, tie waste bags up and put into the main waste bin
- use a ‘swan neck’ technique for closure of the bag and label with date and location as per local policy
- a ‘swan neck’ is a way of closing bag by tying in a loop and securing with a zip tie or tape to make a handle
- clean waste bins regularly with a general purpose neutral detergent
- remove PPE and perform hand hygiene when you have finished handling waste
 Read the safe disposal of waste literature review to find out more about why we do things this way when dealing with waste.
Read the safe disposal of waste literature review to find out more about why we do things this way when dealing with waste.
10. Occupational Safety: Prevention and Exposure Management (including sharps)
 All care homes should have policies in place to ensure that staff are protected from occupational exposure to microorganisms (germs), particularly those that may be found in blood and body fluids.
All care homes should have policies in place to ensure that staff are protected from occupational exposure to microorganisms (germs), particularly those that may be found in blood and body fluids.
Important words and what they meanOccupational exposure is exposure of staff to blood or body fluids in the course of their work.A sharp is a device or instrument such as needles, lancets and scalpels which are necessary for the exercise of specific healthcare activities and are able to cut, prick and/or have the potential to cause injury.Safety device or safer sharp is a medical sharps device which has been designed to incorporate a feature or mechanism that minimises and/or prevents the risk of accidental injury. Other terms include (but are not limited to) safety devices, safety-engineered devices and safer needle devices.
The Health and Safety (Sharp Instruments in Healthcare) Regulations (2013) outline the regulatory requirements for employers and contractors in the healthcare sector in relation to:
- arrangements for the safe use and disposal of sharps
- provision of information and training to employees
- investigations and actions required in response to work related sharps injuries
Safe management of sharps in the care home
Sharps handling must be assessed, kept to a minimum and eliminated if possible with the use of approved safety devices.
Sharps safety
- Always dispose of needles and syringes as a single unit immediately at the point of use.
- Always assemble and label sharps containers correctly as per manufacturers instructions.
- Always use the temporary closure mechanisms on sharps containers in between use.
- Always follow manufacturers’ instructions for safe use and disposal.
- Never re-sheath used needles or lancets.
- Never store sharps containers on the floor.
- Never allow access of sharps containers to residents or the public.
- Never fill sharps containers more than three-quarters full.
Significant occupational exposure
A significant occupational exposure is when someone is injured at work from using sharps or exposed to risk from blood or body fluids which may then result in a blood borne virus (BBV) or other infection.
Examples of this would be:
- a percutaneous injury for example injuries from needles, instruments, bone fragments, or bites which break the skin
- exposure of broken skin for example abrasions, cuts, eczema
- exposure of mucous membranes including the eye from splashing of blood or other high risk body fluids
If you think or know you have had a significant occupational exposure you should:
- report this immediately to the designated person in your care home, this is a legal requirement
- follow the local agreed process for management of an occupational exposure incident and follow the management of occupational injuries flow chart
Resources
 Read the management of occupational exposure to Blood Borne Viruses (BBVs) literature review to find out more about why we do things this way for occupational exposure.
Read the management of occupational exposure to Blood Borne Viruses (BBVs) literature review to find out more about why we do things this way for occupational exposure.

The management of occupational exposure incidents flowchart should be used within your care home so you know what to do for an occupational exposure.
Select the image for full size
Transmission based precautions (TBPs)
In certain circumstances using standard infection control precautions (SICPs) won’t be enough to stop an infection spreading and you will need to use some extra precautions. These extra precautions are called Transmission Based Precautions or TBPs.
Clinical judgement and decisions should be made by staff to determine the necessary IPC precautions required (the local IPCT and/or the HPT should be contacted for advice and support where required).
Clinical judgement and decisions should be based on the:
- suspected or known infectious agent
- transmission route of the infectious agent
- care setting and procedures undertaken
- severity of the illness caused
When TBPs should be used
TBPs should be used if a resident has a suspected or known infection or colonisation.
Important words and what they meanColonisation is the presence of microorganisms on a body surface (such as the skin, mouth, intestines or airway) that does not cause disease in the person or signs of infection.
Infection transmission routes
Infections can be transmitted or spread by:
- contact with microorganisms (germs) on hands or from contaminated equipment or environment
- droplet infection by inhaling infectious droplets, for example flu or COVID-19
- aerosol infection which are inhaled or directly contaminate a mucosal surface or conjunctivae (eyes, nose, and mouth)
Different transmission routes need different TBPs
TBPs are categorised by the route of transmission of infectious agents (some infectious agents can be transmitted by more than one route). Appendix 11 provides details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required. Application of TBPs may differ depending on the setting and the known or suspected infectious agent.
Contact precautions are used to prevent infections that spread through direct contact with the resident or indirectly from the resident’s immediate care environment and care equipment. This is the most common route of cross-infection transmission.
Droplet precautions are used to prevent and control infections spread over short distances (at least 3 feet or 1 metre) via small droplets from the respiratory tract of one individual directly onto the mucosal surface of another person’s mouth or nose or eyes. Droplets penetrate the respiratory system to above the alveolar level.
Airborne precautions are used to prevent and control infections spread without necessarily having close contact via from the respiratory tract of one individual directly onto the surface of another person’s mouth or nose or eyes. Aerosols penetrate the respiratory system to deep into the lung.
Different infections need different TBPs
You might have heard of some infections like norovirus, Meticillin-resistant Staphylococcus aureus (MRSA), Clostridioides. difficile (C.diff/CDI) and flu but there are lots of others.
You can find out more information about the infection the individual has and the precautions you should use in Appendix 11 and/or A-Z of pathogens in the NIPCM.
You can also contact your local IPCT or HPT for further advice if required.
Before using transmission based precautions you need to find out:
- what the suspected or known infection/colonisation is?
- how is it transmitted?
- how severe is the resident’s illness?
- what is the care setting and required procedures?
There are different ways you can find out if a resident has an infection that needs TBPs to be put in place. You can get information about a resident’s infection status from:
- their GP
- local health protection team
- local infection prevention and control team
- laboratory
- hospital or care homes staff from where the resident has been discharged or transferred
Local processes should be followed when obtaining this information.
![]() Further information on transmission based precautions can be found in the definitions of Transmission Based Precautions literature review.
Further information on transmission based precautions can be found in the definitions of Transmission Based Precautions literature review.
1. Resident placement/assessment for infection risk
All residents require to be regularly monitored for infection throughout their stay for the correct IPC precautions to be put in place to minimise the risk of infection being spread.
Residents may be an infection risk if they have:
- diarrhoea, vomiting, an unexplained rash, fever or respiratory symptoms
- a known (laboratory confirmed) or suspected infectious pathogen for which appropriate duration of precautions as outlined in A-Z of pathogens are not yet complete
- been previously positive with a Multi-drug Resistant Organism (MDRO) for example Meticillin-resistant Staphylococcus aureus (MRSA); Carbapenemase Producing Enterobacterales (CPE)*
*CPE should be considered if the resident meets any of the following criteria within the 12-month period before admission:
- been an inpatient in a hospital outside of Scotland
- received holiday dialysis outside of Scotland
- been a close contact of a person who has been colonised or infected with CPE.
See the CPE toolkit for non-acute settings for further information and requirements.
Staff should do the following if any resident displays signs and/or symptoms of infection:
- obtain advice on the resident’s clinical management from their GP and advice on appropriate IPC management from either the local HPT or IPCT
- make resident placement decisions based on advice received or sound judgement by clinical staff who are involved in the resident’s management
- advise the ambulance service of the resident’s infectious condition if transport to hospital is required
Residents should not be moved within the care home if they have signs and symptoms of infection unless essential.
Resident isolation requirements within the care home
Residents may require to be isolated in their own room because of a known or suspected infection. During this time it is important that:
- residents remain in their rooms whilst considered infectious and the door should remain closed. If it is not possible for safety reasons, for example the resident has dementia, an individual risk assessment should be done and any decisions or actions should be documented. The local HPT or IPCT should be contacted for advice
- suitable discrete signage is placed on the door advising others not to enter the room
- there should be as much consistency in staff allocation as possible to care for residents in isolation room areas as an additional IPC measure. This is known as ‘staff cohorting’
- resident isolation requirements should remain under continuous review considering individual risk factors and the impact on the resident. The local HPT or IPCT should be contacted for advice in these circumstances
Note: If a resident requires isolation because of infection or in an outbreak situation, this should be individually risk assessed to ensure the safety and health and wellbeing needs of the resident. Isolation periods must be monitored on daily basis and be for the minimum period specified.
 Read the patient placement, isolation and cohorting literature review to find out more about why we do things this way for resident placement for TBPs.
Read the patient placement, isolation and cohorting literature review to find out more about why we do things this way for resident placement for TBPs.
2. Safe management of care equipment in an isolation room
Cleaning and decontamination of care equipment is essential to reduce the spread of infection when infection is confirmed/suspected.
When dealing with the equipment used in the resident’s isolation room staff should:
- use single use or dedicated reusable care equipment, for example commodes, for the resident in isolation where possible
- clean and decontaminate all care equipment after each use as per Appendix 7
 Read the management of care equipment literature review to find out more about why we do things this way for patient care equipment for TBPs.
Read the management of care equipment literature review to find out more about why we do things this way for patient care equipment for TBPs.
3 - Safe management of the care environment
Isolation room cleaning
Staff should:
- clean and decontaminate the isolation room at least daily or more frequently if advised to do so. If you have been advised to clean more than daily this should be documented in the environmental cleaning schedule
- clean frequently touched surfaces like door handles, bed frames and bedside cabinets at least twice daily
- use correct cleaning products which are either:
a combined detergent/disinfectant solution at a dilution of 1,000 parts per million available chlorine (ppm available chlorine (av.cl.));
or
a general purpose neutral detergent in a solution of warm water followed by disinfection solution of 1,000ppm av.cl.
- follow manufacturers guidance and instructions on how to use the product and what the recommended contact time is for the product to work. This may include rinsing off the disinfection solution to prevent damage to surfaces.
Do not refill spray containers for cleaning products as there is a risk of contamination.
Terminal clean
A terminal clean is carried out when the resident is no longer considered infectious and/or when the environment is cleaned/decontaminated to ensure it is safe for a new resident.
A terminal clean is carried out by:
- removing all healthcare waste and other disposable items from the room
- removing bedding, curtains (bagged before removal from the room) and then wash as infectious linen
- cleaning and decontaminating all reusable care equipment in the room (prior to removal from the room)
The room should then be decontaminated using either:
- a combined detergent disinfectant solution at a dilution (1,000ppm av.cl.) or
- a general purpose neutral detergent clean in a solution of warm water followed by disinfection solution of 1,000ppm av.cl.
The room should be cleaned from the highest to lowest point and from the least to most contaminated point.
Manufacturers’ guidance and recommended product "contact time" should be followed for all cleaning/disinfection solutions.
 Appendix 7 is a poster flowchart for decontamination of reusable non-invasive care equipment that you may wish to print off and place in the care home.
Appendix 7 is a poster flowchart for decontamination of reusable non-invasive care equipment that you may wish to print off and place in the care home.
Note: When an organisation use products or adopts practices that differ from those stated in this manual, that individual organisation is responsible for ensuring safe systems of work including the completion of risk assessments approved through local governance procedures.
4. Personal Protective Equipment (PPE): Respiratory Protective Equipment (RPE)
In addition to PPE used for Standard Infection Control Precautions, appendix 16 of the NIPCM outlines what type of PPE and RPE you will need to wear for infections spread by different transmission routes.
Gloves
Gloves are a single-use item and should be donned immediately prior to exposure risk and should be doffed immediately after each use or upon completion of a task.
Gloves should:
- be worn when exposure to blood, body fluids, (including but not limited to secretions and/or excretions), non-intact skin, lesions and/or vesicles, mucous membranes, hazardous drugs, and chemicals for example cleaning agents, is anticipated/likely
- never be worn inappropriately in situations such as to go between residents, move around a care area, work at IT workstations
- be changed if a perforation or puncture is suspected or identified
- be appropriate for use, fit for purpose and well-fitting
- not be worn as a substitute to hand hygiene
- never be decontaminated with ABHR
Resources
 For appropriate glove use and selection see the flowchart poster which may be printed off and placed in the care home.
For appropriate glove use and selection see the flowchart poster which may be printed off and placed in the care home.
![]() Further information can be found in the Gloves literature review.
Further information can be found in the Gloves literature review.
Aprons/gowns
An apron should be worn when caring for residents known or suspected to be colonised/infected with antibiotic resistant bacteria including contact with the resident’s environment.
Plastic aprons should be used in care home settings for protection against contamination with blood and/or body fluids.
A fluid repellent gown should be used if excessive splashing or spraying is anticipated.
A full body fluid repellent gown should be worn when conducting AGPs on residents known or suspected to be infected with a respiratory infectious agent.
![]() Further information can be found in the Aprons/Gowns literature review.
Further information can be found in the Aprons/Gowns literature review.
Eye/face protection
A face visor or goggles should be used in combination with a fluid resistant Type IIR surgical mask when caring for symptomatic residents infected with droplet transmitted infectious agents.
A face visor or goggles should be used in combination with a fluid resistant FFP3 respirator when caring for symptomatic residents infected with an airborne transmitted infectious agent.
Eye/face protection should be worn:
- by all of those in the room if potentially infectious AGPs are conducted
- for the care of residents with novel infectious agents including pandemic influenza
 Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Surgical masks
A Type IIR fluid resistant surgical mask (FRSM) should be worn when caring for a resident with a suspected/confirmed infectious agent spread by the droplet route.
FRSMs should be worn (where tolerated) by residents with suspected/confirmed infectious agents spread by the droplet or airborne routes, as a form of source control and should meet type II or IIR standards.
 Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Read Appendix 11 for details of the type of precautions, optimal resident placement, isolation requirements and any respiratory precautions required.
Respiratory Protective Equipment (RPE)
PPE should still be used in accordance with SICPs when using respiratory protective equipment (RPE). See Chapter 1.4 for PPE use for SICPs.
The use of FFP3s is governed by health and safety regulations and they must be fit tested to the user to ensure the required protection is provided.
The Health and Safety Executive (HSE) provides information regarding fitting and fit checking of RPE.
Respiratory Protective Equipment (RPE), for instance FFP3 and facial protection, should be considered when:
- a resident is admitted or develops a known/suspected infectious agent/disease spread wholly by the airborne route
- carrying out AGPs on residents with known/suspected infectious agent spread wholly or partly by the airborne or droplet route
FFP3 respirators
It is an HSE requirement that staff who need to wear an FFP3 respirator must be fit tested.
FFP3 respirators should not be worn by staff who are not trained in their use or who have not been fit tested.
All FFP3 respirators must be:
- fit tested (by a competent fit test operator) on all staff who may be required to wear a respirator to ensure an adequate seal/fit according to the manufacturers’ guidance
- fit checked (according to the manufacturers’ guidance) every time a respirator is donned to ensure an adequate seal has been achieved
- single-use (disposable) and fluid resistant
- compatible with other facial protection used such as protective eyewear so that this does not interfere with the seal of the respiratory protection. Regular corrective spectacles are not considered adequate eye protection
- put on before entry into the resident’s room and removed in a safe area once outside the resident’s room
- changed after each use
Signs that a change in respirator is required include:
- breathing becomes difficult
- the respirator is wet or moist
- the respirator is damaged
- the respirator is obviously contaminated with body fluids such as respiratory secretions
Resources
 A poster containing information on compatibility of facial hair and FFP3 respirators can be used when fit testing and fit checking.
A poster containing information on compatibility of facial hair and FFP3 respirators can be used when fit testing and fit checking.
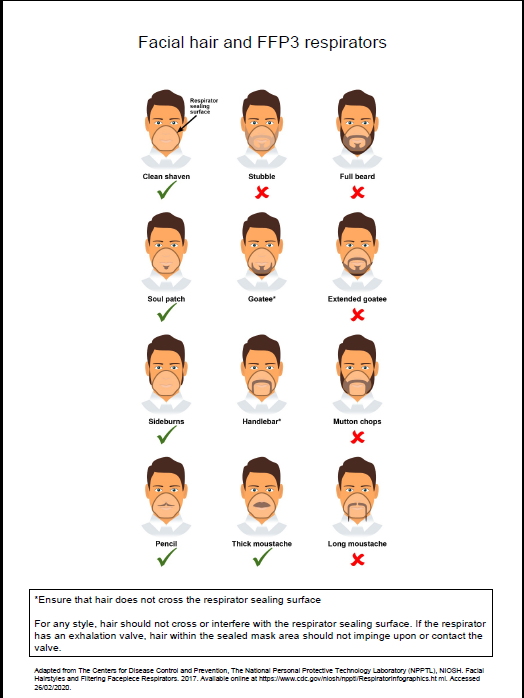
![]() Further information regarding fitting and fit checking of respirators can be found from the Health and Safety Executive
Further information regarding fitting and fit checking of respirators can be found from the Health and Safety Executive
Aerosol Generating Procedure (AGP)
An AGP is a medical procedure that can result in the release of airborne particles from the respiratory tract and is associated with an increased risk of transmission when treating someone who is suspected or known to be suffering from an infectious agent transmitted wholly or partly by the airborne or droplet route.
The most common AGPs undertaken in the Care Home Setting are Continuous Positive Airway Pressure Ventilation (CPAP) or Bi-level Positive Airway Pressure Ventilation (BiPAP) or tracheostomy procedures (insertion or removal) and open suctioning beyond the oro-pharynx.
The full list of medical procedures that have reported to be aerosol generating and are associated with an increased risk of respiratory transmission can be found in appendix 17.
A poster is also available on PPE when undertaking AGPs within health and social care settings.
Rooms should always be decontaminated following an AGP. Clearance of infectious particles after an AGP is dependent on the ventilation and air change within the room. In an isolation room with mechanical ventilation 10-12 air changes per hour (ACH) a minimum of 20 minutes is required; in a side room with 6 ACH this would be approximately one hour.
It is often difficult to calculate air changes in areas that have natural ventilation only, meaning no mechanical ventilation. Natural ventilation, particularly when reliant on open windows can vary depending on the climate. An air change rate in these circumstances has been agreed as 1-2 air changes/hour.
Rooms should always be decontaminated following the completion of an AGP. Regardless of the number of air changes, a period of 10 minutes should pass to allow larger droplets to settle before the room can be cleaned. Staff are required to wear the appropriate PPE until the fallow time has been met.
Resources
![]()
For further information on fallow times refer to Table 1 in Appendix 17.
 Further information can be found in the literature reviews aerosol generating procedures, Respiratory Protective Equipment (RPE), Personal Protective Equipment (PPE) for Infectious Diseases of High Consequence (IDHC)
Further information can be found in the literature reviews aerosol generating procedures, Respiratory Protective Equipment (RPE), Personal Protective Equipment (PPE) for Infectious Diseases of High Consequence (IDHC)
Post AGP fallow time (PAGPFT)
Time is required after an AGP is performed to allow the aerosols still circulating to be removed/diluted. This is referred to as post AGP fallow time (PAGPFT) and is a function of the room ventilation air change rate.
The post aerosol generating procedure fallow time (PAGPFT) calculations are detailed in appendix 17. It is often difficult to calculate air changes in areas that have natural ventilation only.
If the area has zero air changes and no natural ventilation, then AGPs should not be undertaken in this area.
The duration of AGP is also required to calculate the PAGPFT and clinical staff are therefore reminded to note the start time of an AGP. It is presumed that the longer the AGP, the more aerosols are produced and therefore require a longer dilution time. During the PAGPFT staff should not enter this room without FFP3 masks. Other residents, other than the resident on which the AGP was undertaken, should not enter the room until the PAGPFT has elapsed and the surrounding area has been cleaned appropriately. As a minimum, regardless of air changes per hour (ACH), a period of 10 minutes should pass before rooms can be cleaned. This is to allow for the large droplets to settle. Staff should not enter rooms in which AGPs have been performed without airborne precautions for a minimum of 10 minutes from completion of AGP. Airborne precautions may also be required for a further extended period of time based on the duration of the AGP and the number of air changes. Cleaning can be carried out after 10 minutes regardless of the extended time for airborne PPE.
Contact your local HPT/IPCT if further advice is required.
 Read the RPE literature review to find out more about why we do things this way for respiratory protective equipment.
Read the RPE literature review to find out more about why we do things this way for respiratory protective equipment.
Use of FFP3 respirators
- Where staff have concerns, they may choose to wear an FFP3 respirator rather than a fluid-resistant surgical mask (FRSM) when providing patient care, provided they are fit tested. This is a personal PPE risk assessment.
5. Infection prevention and control during care of the deceased
If a resident dies when in the care home SICPs and TBPs should still be applied. This is due to the ongoing risk of infectious transmission via contact although the risk is usually lower than for the living.
It is important that information on the infection status of the deceased is sought and communicated at each stage of handling and risk assessments performed.
Viewing, washing and/or dressing of the deceased see Appendix 12 - Application of infection prevention precautions in the deceased for guidance on the precautions required and what is permitted for certain types of infections.
Staff should advise relatives of the appropriate precautions to be taken when viewing and/or having physical contact with the deceased, including when this should be avoided.
 Read the infection prevention and control during care of the deceased literature review to find out more about why we do things this way when dealing with the deceased.
Read the infection prevention and control during care of the deceased literature review to find out more about why we do things this way when dealing with the deceased.
Care home appendices
These appendices from the NIPCM can be used in care homes.
Appendix 5 - Glove use and selection
Appendix 6 - Putting on and removing PPE
Appendix 7 - Decontamination of reusable care equipment
Appendix 8 - Management of linen at care level
Appendix 9 - Management of blood and body fluid spillages
Appendix 10 - Management of occupational exposure incidents
Appendix 12 - Application of infection control precautions in the deceased
Appendix 18 - Hierarchy of controls
Care home resources
The resources section can be used as supporting tools for the Care Home Infection Prevention and Control Manual (CH IPCM).
- Aerosol Generating Procedures
- HAI Compendium
- Hand hygiene
- Gastro-intestinal illness
- Information leaflets.
These leaflets are also available in different languages National Infection Prevention and Control Manual: Information Leaflets - language translations (scot.nhs.uk)- Clostridiodes difficile (CDI) - Information for people who are getting care, their visitors, and anyone else who is in a care setting
- Group A Streptoccocal infection - information for patients
- Healthcare associated infection (HAI) - Information for the public
- Vancomycin-resistant enterococci VRE - Information for patients
- Washing clothes at home - Information for people in
hospitals or care homes and their relatives
- Respiratory hygiene
- Respiratory illness
- Transmission Based Precautions
- World Hand Hygiene Day 5 May 2023 - Accelerate action together. SAVE LIVES clean your hands
How to contact us
If you have any questions or feedback about the Care Home IPCM then you can contact us by email or telephone.
Telephone: 0141 300 1175
COVID-19 NIPCM Archives
This page links to the following archived COVID-19 guidance that was in the NIPCM:
- Acute addendums
- Community addendums
- Care Home addendums
- Appendix 21 - COVID-19 Pandemic controls for Acute Settings including Scottish Ambulance Service
- Appendix 22 - Community Infection Prevention and Control COVID-19 Pandemic
- Appendix 21 - COVID-19 Pandemic controls for health and care settings
- Hospital Testing Tables
COVID-19 Acute Addendum Archives
Version |
Date |
Summary of changes |
|
26/10/2020 |
First publication |
|
|
28/10/2020 |
Update to section 5.7 ‘Safe Management of the Care Environment’ to reflect detail of 2nd daily clean. Update to section 5.5 ‘Personal Protective Equipment’ to be more explicit. |
|
|
06/11/2020 |
Update to align references to changing of facemasks between pathways. |
|
|
20/11/2020 |
New section on communications when transferring a suspected/confirmed case New section on car sharing New section on visiting Update to definition of recovered patient |
|
|
09/12/2020 |
New section on PPE requirements for delivery of vaccinations New section on outbreaks |
|
|
17/12/2020 |
New section on COVID-19 testing New section on Patients returning from weekend/day pass New section on Whole Genome Sequencing (WGS) Link to RCPCH paediatric guidance for pre-operative admission assessment and testing requirements New FRSM poster (ways to improve fit) |
|
|
23/12/2020 |
Update to 5.0.3 to reflect changes in stepdown guidance Inclusion of SG link to asymptomatic staff testing information New section on 5.1.1 Non-COVID patient transfers between different wards and hospitals |
|
|
22/01/2021 |
Update to the COVID-19 testing section and associated testing table New section on guidance for the Discontinuation of Infection control precautions and discharging COVID-19 patients from hospital Update to PPE guidance specifically in relation to visors New section on the hierarchy of controls |
|
|
18/02/2021 |
Update to resources and Rapid reviews content Additional wording added to definition of suspected case section to reflect wide variety of presenting symptoms Strengthening of triage question relating to travel history Additional paragraph in PPE section reinforcing need for visiting staff to seek clarity on patient pathway and PPE requirements prior to patient contact |
|
|
26/03/2021 |
Sessional PPE use no longer accepted beyond eye protection in the high risk pathway and FRSMs across all pathways. Update to stepdown requirement for inpatient table to recognise need for clinical assessment Useful tools section |
|
|
07/05/2021 |
Environmental risk assessment |
|
|
14/05/2021 |
Change to AGP list to remove upper airway suctioning during Upper GI Endoscopy and replace with suctioning beyond the oro-pharynx. |
|
|
18/05/2021 |
Update to COVID-19 testing table to reflect the need to test all contacts of confirmed cases. |
|
|
25/06/2021 |
Update to PPE table to emphasise Risk Assessment in low and medium risk pathway Addition of risk associated with valved respirators Change in controls for management of linen, waste and environmental cleaning from TBPs to SICPs within the Medium Risk pathway |
|
|
8/7/2021 |
5.2 COVID-19 testing. Update made to include 'or the first positive test, if asymptomatic or other symptoms, unless they develop new possible COVID-19 symptoms' regarding any patient who has previously tested positive for SARS-CoV-2 by PCR. 5.3.8 Update to table 2 - stepdown table for 'Patient discharging to a care facility including nursing homes and residential homes' 5.3.8 Inclusion of section on 'Patients discharged from hospital to a care home (non-COVID-19) |
|
|
19/7/2021 |
Update to Hierarchy of control including risk assessment algorithm Inclusion of a specific paragraph advising on the use of FFP3 masks |
|
|
30/8/2021 |
Update to physical distancing |
Scottish COVID-19 Infection Prevention and Control Addendum for Community Health and Care Settings
Version |
Date |
Summary of changes |
|
07/01/2021 |
First version |
|
|
25/01/2021 |
Addition of section 7.2.5 'Discontinuing IPC control measures in community health and care settings for COVID-19 individuals' |
|
|
31/03/2021 |
Health Centres included in list |
|
|
08/07/2021 |
7.5.5 Change to AGP list to remove upper airway suctioning during Upper GI Endoscopy and replace with suctioning beyond the oro-pharynx. |
|
|
25/08/2021 |
Inclusion of dental services within the addendum |
|
|
31/08/2021 |
Update to physical distancing |
|
|
15/09/2021 |
Update to physical distancing to include further information for visitors and residents within residential homes. |
COVID-19 Care Home Addendum Archive
Version |
Date |
Summary of changes |
|
16/12/2020 |
First version |
|
|
25/01/2021 |
Inclusion of new section 6.2.4 'Discontinuing IPC precautions in care homes for residents who are COVID-19 positive' |
|
|
31/03/2021 |
6.1.2 Definition of suspected case; Additional information and links included. |
|
|
8 July 2021 |
6.1.3 Triaging of residents admitted to a care home updated with changes to testing and self-isolation |
|
|
31/08/2021 |
Updates to physical distancing |
Respiratory Addendum archive
Version |
Date |
Summary of changes |
|
29/11/2021 |
Guidance launched |
|
|
13/12/2021 |
Update to ‘Determining the IPC precautions required for AGPs’ |
|
|
17/01/2022 |
Addition of advice for regular testing in critical care units where AGPs are regularly performed on the non respiratory pathway. Reduction of COVID-19 duration of precautions from 14 days to 10 days. |
|
|
20/01/2022 |
Update to Non COVID-19 discharges (non respiratory pathway) from hospitals to care homes Addition of sections for primary care and care homes to reinforce and support assessment using the hierarchy of controls. |
|
|
03/02/2022 |
Additional information for visitors entering AGP zones. |
|
|
23/02/2022 |
Risk assessment for management of patient placement in long term residential community settings (section 5.8 and section 5.12.2) Update to hospital testing table |
|
|
01/04/2022 |
The following updates reflect changes to healthcare COVID-19 pandemic controls as outlined in DL (2022) 07 as follows; Changes to patient testing requirements including Hospital Testing Table Inclusion of the wider use of Rapid Diagnostic Testing (including POCT) or LFD testing Changes to management of contacts including inclusion of 28 day contact exemption Changes to respiratory screening questions Changes to testing requirement pre AGP on the non respiratory pathway Withdrawal of car sharing guidance Removal of physical distancing guidance Please note: the above changes within version 1.6 are not applicable in care homes, prisons and social community and residential care settings at the time of version update; Extant guidance remains in place for these settings. |
|
|
07/04/2022 |
Update to include definition of fully vaccinated Addition to physical distancing noting that services may choose to retain physical distancing where they deem it necessary |
|
|
27/04/2022 |
Addition of testing responsibilities at an organisational level and clarity of testing language Change to isolation advice for service users with COVID-19 Removal of vaccination as part of contact management. |
Appendix 21 -COVID-19 Pandemic Controls for Acute NHS settings including Scottish Ambulance Service (SAS) Archive
Version |
Date |
Summary of changes |
|
10/05/2022 |
First publication – Marks transition from Winter Respiratory Infection IPC Addendum back to NIPCM. |
|
|
30/05/2022 |
Reference to COVID-19 screening removed. |
|
|
13/07/2022 |
Addition of dental services and GPs to title. |
|
|
28/07/2022 |
Removal of GPs in title as now included in Appendix 22. |
|
|
22/08/ 2022 |
Changes made to testing requirements in line with DL 2022(29) issued on 22nd August 2022 |
|
|
16/09/2022 |
Update following Directors Letter (2022)32 - pause in asymptomatic COVID-19 testing in health and social care |
|
|
28/09/2022 |
Removal of ‘Primary Care Settings’ from Table 2 – Respiratory Screening Questions |
|
|
06 /10/ 2022 |
Broken links replaced and update to COVID-19 testing requirements in line with Directors Letter (2022)32 |
|
|
18/11/2022 |
Updated to reflect that the advice contained within the Scottish Government’s DL(2022)10 remains extant. |
Appendix 22 - Community Infection Prevention and Control COVID-19 Pandemic Archive
Version |
Date |
Summary of changes |
|
29/06/2022 |
First publication – Marks transition from Winter Respiratory Infection IPC Addendum to a Community COVID-19 Pandemic Appendix. |
|
|
28/07/2022 |
GP surgeries included in this this appendix and removed from Appendix 21 – COVID-19 acute settings |
|
|
16/09/2022 |
Content revised to reflect SG Extended Use of Facemasks Policy for ASC settings. |
|
|
04/10/2022 |
Link added to revised content from SG clarifying use of facemasks in social care settings by healthcare staff |
|
|
18/11/2022 |
Updated to reflect that the advice contained within the Scottish Government’s DL(2022)10 remains extant. |
Appendix 21 - COVID-19 Pandemic IPC Controls for Health and Social Care Settings Archive
Version |
Date |
Summary of changes |
|
20/03/2023 |
New appendix which combines content from COVID-19 Appendix 21 for acute settings and Appendix 22 for community settings into a single pandemic appendix for health and social care settings. |
|
|
16/05/2023 |
Amendments to content made following Withdrawal of the Coronavirus (COVID-19): Extended Use of Face Masks and Face Coverings Guidance Across Health and Social Care Scottish Government DL (2023) 11. Renumbered as Appendix 19 on 2 June 2023 due to the archiving of outdated COVID-19 appendices. |
Hospital testing tables archive
Version |
Date |
Summary of changes |
|
23/12/2020 |
First version produced by Scottish Government |
|
|
22/02/2021 |
ARHAI Scotland taking responsibility for producing table. Inclusion of frontpage and review of content undertaken. |
|
|
18/05/2021 |
Update made to testing requirement 3 regarding emergency admissions and PCR/POCT testing. Update made to requirement 7 Transfer of a non COVID-19 patient to another hospital/NHS board about transferring patient while waiting for test results. Update to section Testing Contacts of confirmed COVID-19 cases. |
|
|
06/09/2021 |
Updates to sections on staff testing. Reference to household member testing positive removed. |
|
|
01/12/2021 |
Updated to be in line with the respiratory addendum. |
|
|
02/12/2021 |
Update to frontpage reference to discharge to care homes to include for those still in the 14 day isolation period. |
|
|
21/12/2021 |
Update to frontpage to include definition of admissions. Update to testing prior to an AGP to include further information on negative tests before an AGP. |
|
|
23/02/2022 |
Addition of relevant policy letters or guidance relevant to each testing recommendation. |
|
|
01/04/2022 |
Updates to reflect changes to healthcare COVID-19 pandemic controls outlined in DL (2022) 07 as follows
|
|
|
07/04/2022 |
Clarity relating to COVID-19 testing terminology |
|
|
25/04/2022 |
Additional clarifications relating to COVID-19 testing terminology |
|
|
10/05/2022 |
Changes to reflect transition of Winter Respiratory IPC addendum to COVID-19 appendix |
|
|
22/08/2022 |
Changes made to testing requirements in line with DL 2022(29) issued on 22nd August 2022 |
|
|
16/9/2022 |
Testing requirements updated with new paragraphs on symptomatic and asymptomatic testing. Addition of Appendix 1- List of PCR-based and non-PCR based tests in use in Scotland |
|
|
06/10/2022 |
Update to duration of precautions to reference NIPCM and A-Z |
References
- Reference 1
The use of the word 'Persons' can be used instead of ‘Patient’ when using this document in non-healthcare settings.
Glossary
- Abrasion
A graze. A minor wound in which the surface of the skin or a mucous membrane has been worn away by rubbing or scraping.
- Acute care setting/Acute hospital
This is a unique, demanding and fast-paced environment designed to accommodate a wide variety of urgent, or emergent patient care needs.
- Adverse event
An event that could have caused or did result in harm to people or groups of people.
- Aerosol Generating Procedures (AGPs)
An AGP is a medical procedure that can result in the release of airborne particles from the respiratory tract when treating someone who is suspected or known to be suffering from an infectious agent transmitted wholly or partly by the airborne or droplet route.
- Aerosols
- Airborne (aerosol) transmission
The spread of infection from one person to another by airborne particles (aerosols) containing infectious agents.
- Airborne particles (aerosols)
Very small particles (of respirable size) that may contain infectious agents. They can remain in the air for extended periods of time and can be carried over long distances by air currents. Aerosols can be released during aerosol generating procedures (AGPs).
- Airborne precautions
A group of transmission-based precautions to prevent the spread of airborne pathogens.
- Alcohol based hand rub (ABHR)
A gel, foam or liquid containing one or more types of alcohol that is rubbed into the hands to inactivate microorganisms and/or temporarily suppress their growth.
- Alert organism
An organism that is identified as being potentially significant for infection prevention and control practices. Examples of alert organisms include Meticillin Resistant Staphylococcus aureus (MRSA), Clostridioides difficile (C.diff) and Group A Streptococcus.
- Alveolar
Refers to the alveoli which are the small air sacs in the lungs. Alveoli are located at the ends of the air passageways in the lungs, and are the site at which gas exchange takes place.
- Anteroom
An area with a door from/to the outside corridor and a second door giving access to the patient area (where both doors will never be open at the same time).
- Antimicrobial
An agent that kills microorganisms, or prevents them from growing.
Antimicrobials are grouped according to the microorganisms they act against, such as, antibiotics, antivirals, antifungals and antiparasitics.
- Antimicrobial hand wipes
Hand wipes that are moistened with an antimicrobial solution/agent at a concentration sufficient to inactivate microorganisms and/or temporarily suppress their growth.
- Antimicrobial resistance
The ability of a microorganism to resist the action of an antimicrobial drug/agent which previously could treat the infection caused by that microorganism.
- Antisepsis
The process of preventing infection by inhibiting the growth and multiplication of infectious agents. This is usually achieved by application of a germicidal preparation known as an antiseptic.
- Aseptic Technique
A healthcare procedure designed to minimise the risks of exposing the person being cared for to pathogenic micro-organisms during simple (e.g dressing wounds) and complex care procedures (e.g. surgical procedures).
- Asymptomatic
Not showing any symptoms of disease but where an infection may be present.
- Augmented Care
In the context of infection prevention and control, most care designated as augmented will be that where medical/nursing procedures render the patients susceptible to invasive disease from environmental and opportunistic pathogens. However, there is no fixed definition of ‘augmented care’.
- Autoclave
Machine used for sterilising re-usable equipment using steam sterilisation. Re-usable equipment is exposed to steam at a required temperature, pressure, and time.
- Bay
A partly enclosed area within a ward containing one bed (single bay) or multiple beds (multi-bed bay).
- Blood Borne Viruses (BBV)
Viruses carried or transmitted by blood, for example Hepatitis B, Hepatitis C and HIV.
- Body Fluids
Fluid produced by the body such as urine, faeces, vomit or diarrhoea.
- British Standards (BS), European Standards (EN) and International Standards (ISO)
National standards specify the requirements for application in the particular country.
- BS denotes Britain's National Standards which are controlled by the British Standards Institute (BSI)
- EN denotes a Standard which is adopted by the European community and is controlled by the European Committee for Standardisation (CEN). Once a European Standard has been agreed it supersedes any existing national standard and becomes the new national standard. In Britain these Standards are then prefixed with BS EN
- ISO denotes a worldwide standard issued by the International Organisation for Standardisation. Once an International Standard has been adopted as a European Standard it supersedes the existing European standard. In Britain these Standards are then prefixed with BS EN ISO
- Care setting
Includes but is not limited to general practice, dental and pharmacy (primary care), acute-care hospitals, emergency medical services, urgent-care centres and outpatient clinics (secondary care), specialist treatment centres (tertiary care), long-term care facilities such as nursing homes and skilled nursing facilities (community care), and care provided at home by professional healthcare providers (home care).
- Care staff
Any person who cares for patients, including healthcare support workers and nurses.
- Central Venous Catheter (CVC)
An intravenous catheter that is inserted directly into a large vein in the neck, chest or groin to give intravenous drugs, fluids and blood and to allow for quick medical tests.
- Chlorine
A chemical that is used for disinfecting, fumigating and bleaching.
- Cleaning
The removal of any dirt, body fluids (blood, vomit) etc by use of an appropriate cleaning agent such as detergent.
- Clinical wash hand basin
A sink designated for hand washing in clinical areas.
- Cohort area
A bay/ward in which a group of patients (cohort) with the same infection are placed. Cohorts are created based on clinical diagnosis, microbiological confirmation when available, epidemiology, and mode of transmission of the infectious agent.
- Colonisation
The presence of microorganisms on a body surface (such as the skin, mouth, intestines or airway) that does not cause disease in the person or signs of infection.
- Conjunctivae
Mucous membranes that cover the front of the eyes and the inside of the eyelids.
- Contact dermatitis
The inflammation of the skin (epidermis and adjacent dermis) resulting from direct contact of a substance that could either be an irritant (irritant contact dermatitis) or allergen (allergic contact dermatitis) with the surface of the skin.
- Contact precautions
Series of procedures/interventions used in addition to routine practices to prevent transmission of infectious agents that spread by direct or indirect contact.
- Contact transmission
The spread of infectious agents from one person to another by contact. When spread occurs through skin-to-skin contact, this is called direct contact transmission. When spread occurs via a contaminated object, this is called indirect contact transmission.
- Contaminated
The presence of an infectious agent on a body surface; also on or in clothes, bedding, surgical instruments or dressings, or other inanimate articles or substances including water and food.
- Cough etiquette/respiratory hygiene
Source control measures intended to contain respiratory secretions in order to limit transmission of respiratory pathogens.
- Cross-infection/Cross-transmission
Spread of infection from one person, object or place to another.
- Decontamination
The process of removing, or killing pathogens on an item or surface to make it safe for handling, re-use or disposal, by cleaning, disinfection and/or sterilisation.
- Detergent
A chemical cleansing agent that can dissolve oils and remove dirt.
- Diarrhoea
Passing looser more frequent stools than is normal for the individual.
- Direct contact transmission
Spread of infectious agents from one person to another by direct skin-to-skin contact.
- Disinfectant
A chemical used to reduce the number of infectious agents from an object or surface to a level that means they are not harmful to health.
- Disinfection
The treatment of surfaces/equipment using physical or chemical means, for example using a chemical disinfectant, to reduce the number of infectious agents from an object or surface to a level at which they are not harmful to health.
- Doffing
To remove (an item of clothing or an item of PPE).
- Domestic waste
Waste produced in the care setting that is similar to waste produced in the home.
- Donning
To put on (an item of clothing or an item of PPE).
- Droplet
A small drop of moisture, larger than airborne particle, that may contain infectious agents. Droplets can be released when a person talks, coughs or sneezes, and during some medical or patient care procedures such as open suctioning and cough induction by chest physiotherapy. It is thought that droplets can travel around 1 metre (3 feet).
- Droplet Nuclei
Droplet nuclei are aerosols formed from the rapid evaporation/desiccation of larger droplet particles when expelled/exhaled from the respiratory tract.
- Droplet transmission
The spread of infection from one person to another by droplets containing infectious agents.
- Emollient
An agent used to soothe the skin and make it soft and supple.
- Enhanced single room (with en-suite facilities and ventilated lobby)
-
- Enhanced single room (with en-suite facilities)
-
- En-suite facilities
En-suite facilities should contain a shower, WC and a general wash-hand basin.
- En-suite single-bed room
A room with space for one patient with en-suite facilities.
- Exceptional infection episode
A single case of an infection that has severe outcomes for an individual patient OR has major infection control/public health implications e.g. infectious diseases of high consequence such as extensively drug resistant tuberculosis (XDR-TB).
- Excretions
Waste products produced by the body such as urine and faeces (bowel movements).
- Exposure
The condition of being exposed to something that may have a harmful effect such as an infectious agent.
- Exposure Prone Procedures (EPPs)
Certain medical and patient care procedures where there is a risk that injury to the healthcare worker may result in exposure of the patient’s open tissues to the healthcare worker’s blood e.g the healthcare worker’s gloved hands are in contact with sharp instruments, needle tips or sharp tissues inside a patient’s body.
- Face covering
A term that applies collectively to items used to cover the nose and mouth. Also referred to as a face mask.
These should not be confused with items of PPE.
- Fallow time
The period of time required for droplets and/or aerosols to settle and be removed from the air following a procedure. It is also known as settle time.
- FFP3
Respiratory protection that is worn over the nose and mouth designed to protect the wearer from inhaling hazardous substances, including airborne particles (aerosols). FFP stands for filtering facepiece. There are three categories of FFP respirator: FFP1, FFP2 and FFP3. An FFP3 respirator or hood provides the highest level of protection, and is the only category of respirator legislated for use in UK healthcare settings.
- Fit check/seal check
A fit check, otherwise known as a user seal check, is a simple and quick method of checking that a respirator has been donned correctly to form a tight seal around the face. Fit checks are not substitutes for, and should not be confused with, fit testing.
- Fit Testing
A method to evaluate how well a tight-fitting respirator fits the wearer and seals adequately to their face. This process verifies the correct model, style, and size of respirator suitable for an individual.
- Fluid resistant surgical mask (FRSM)
- Fluid-resistant
A term applied to fabrics that resist liquid penetration, often used interchangeably with 'fluid-repellent' when describing the properties of protective clothing or equipment.
- Fomites
An inanimate substance or object that can transfer a pathogen to a host.
- Germicide
An agent capable of destroying microorganisms, particularly organisms that are pathogenic.
- GP
General practitioner (your family doctor).
- Group 4 Infections
Definition taken from the HSE Approved list of biological agents www.hse.gov.uk/pubns/misc208.pdf
Group 4 infections cause severe human disease and are a serious hazard to employees; they are likely to spread to the community and there is usually no effective prophylaxis or treatment available.
- Hand Hygiene
The process of decontaminating your hands using either alcohol based hand rub or liquid soap and water.
- Hand rub
A gel, foam or liquid containing one or more types of active ingredient that is rubbed into the hands to inactivate microorganisms and/or temporarily suppress their growth. A hand rub should meet the required British/European Standards as defined in the hand products literature review.
- Health Protection Team (HPT)
A team of healthcare professionals whose role it is to protect the health of the local population and limit the risk of them becoming exposed to infection and environmental dangers. Every NHS board has a HPT.
- Healthcare Associated Infection (HAI)
Infections that occur as a result of medical care, or treatment, in any healthcare setting.
- Healthcare associated infection outbreak
Two or more linked cases associated with the same infectious agent, within the same healthcare setting, over a specified time period; or a higher than expected number of cases in a given healthcare area over a specified time period.
- Healthcare infection data exceedance
A greater than expected rate of infection compared with the usual background rate for the place and time where the incident has occurred.
- Healthcare infection exposure incident
An exposure of patients, staff, or the public to a possible infectious agent, as a result of a healthcare system failure or near misses e.g. ventilation, water or a decontamination incident.
- Healthcare Waste
Waste produced as a result of healthcare activities for example soiled dressings, sharps.
- Hierarchy of controls
This is a systematic process which provides a consistent approach to minimizing or eliminating exposures to hazards in the workplace.
- High Consequence Infectious Disease (HCID)
A High Consequence Infectious Disease (HCID) is defined according to the following criteria:
- causes acute infectious disease
- typically has a high case-fatality rate
- may not have effective prophylaxis or treatment
- difficult to recognise and detect quickly
- ability to spread in the community and within healthcare settings
- requires an enhanced individual, population, and system response for safe, efficient, and effective management
Previously referred to as an Infectious Diseases of High Consequence (IDHC).
- Hospital infection incident assessment tool (HIIAT)
Used by the IPCT or HPT to assess every healthcare infection incident i.e. all outbreaks and incidents including decontamination incidents or near misses in any healthcare setting (that is the NHS, independent contractors providing NHS Services and private providers of healthcare).
- Hygiene Waste
Waste that is produced from personal care. In care settings this includes feminine hygiene products, incontinence products and nappies, catheter and stoma bags. Hygiene waste may cause offence due to the presence of recognisable healthcare waste items or body fluids. It is usually assumed that hygiene waste is not hazardous or infectious.
- Hypochlorite
A chlorine-based disinfectant such as bleach.
- Immunisation
To provide immunity to a disease by giving a vaccination.
- Immunocompromised patient/individual
Any person whose immune response is reduced or deficient, usually because they have a disease or are undergoing treatment. People who are immunocompromised are more vulnerable to infection.
- Impervious
Cannot be penetrated by liquid.
- Incident Management Team (IMT)
A multidisciplinary group with responsibility for investigating and managing an incident.
- Incident/outbreak
An incident/outbreak may be:
- An exceptional infection episode, defined a single case of rare infection that has severe outcomes for an individual AND has major implications for others (patients, staff and/or visitors), the organisation or wider public health for example, high consequence infectious disease (HCID) OR other rare infections such as XDR-TB, botulism, polio, rabies, or diphtheria.
- A healthcare infection exposure incident, defined as exposure of patients, staff, public to a possible infectious agent as a result of a healthcare system failure or a near miss, for example ventilation, water or decontamination incidents.
- A healthcare associated infection outbreak, defined as two or more linked cases associated with the same infectious agent, within the same healthcare setting, over a specified time period, or a higher-than-expected number of cases in a given healthcare area over a specified time period.
- A healthcare infection data exceedance, defined as a greater than expected rate of infection compared with the usual background rate for the place and time where the incident has occurred.
- A healthcare infection near miss incident, which had the potential to expose patients to an infectious agent but did not, for example decontamination failure.
- Indirect contact transmission
The spread of infectious agents from one person to another via a contaminated object.
- Infection
Invasion of the body by a harmful organism or infectious agent such as a virus, parasite, bacterium or fungus.
- Infection Prevention and Control Team (IPCT)
A multidisciplinary team responsible for preventing, investigating and managing an infection incident or outbreak.
- Infectious agent
Any organism, such as a virus, parasite, bacterium or fungus, that is capable of causing an infection or infectious disease.
- Infectious period
The time when an infectious agent may be transmitted directly or indirectly from an infected person to another person. Also known as “period of infectiousness” and “communicability”.
- Inpatient
A patient is termed an inpatient when they occupy a staffed bed in a hospital and either remains overnight (whether intended or not), or is expected to remain overnight but is discharged earlier. An inpatient’s admission can be an emergency, an elective or as a transfer.
- Invasive device
A device which penetrates the body, either through a body cavity or through the surface of the body. Central Venous Catheters (central line), Peripheral Arterial Lines and Urinary Catheters are examples of invasive devices.
- Invasive procedure
A medical/healthcare procedure that penetrates or breaks the skin or enters a body cavity.
- Isolation
Physically separating patients to prevent the spread of infection.
- Isolation Suite/Room
An isolation room/suite consists of enhanced en-suite single bedrooms.
An en-suite single bedroom is defined as: consisting of a bed, locker/wardrobe, clinical wash-hand basin and en-suite shower, WC and wash-hand basin. (In new build, space for a social support zone for overnight stay and a clinical support zone is also provided).
- Enhanced single room (with en-suite facilities), also called isolation room, is the same as an en-suite single-bed room but with a ventilation system that prevents uncontrolled escape of infectious aerosols from the room to adjacent areas. It can also provide a degree of dilution of infectious aerosols in the room for the safety of staff and visitors. The room should have extract ventilation that exceeds its supply, such that gaps in its fabric leak inwards not outwards.
- Enhanced single room (with en-suite facilities and ventilated lobby), also called isolation suite, is the same as an enhanced single room (with en-suite facilities) but with a lobby having positive pressure ventilation.
- J
No terms
- K
No terms
- Lateral Flow Device (LFD)
A test carried out using a small medical device that tests whether or not there is a particular substance, gene, etc. in a sample. For example, to identify those who have COVID-19 but are not presenting symptoms.
- Long Term Care Facility (LTCF)
Long term care facilities provide a variety of services, both medical and personal care, to people who are unable to live independently.
- Mechanical Ventilation
Mechanical ventilation brings fresh air into a building from outside via a controllable method. Basic systems consist of a fan and either collection (extraction) or distribution (supply) ductwork.
- Microorganism (microbe)
Any living thing (organism) that is too small to be seen by the naked eye. Bacteria, viruses and some parasites are microorganisms.
- Mode of transmission
The way that microorganisms spread from one person to another. The main modes or routes of transmission are airborne (aerosol) transmission, droplet transmission and contact transmission.
- Mucocutaneous exposure
An incident in which the mucous membranes (e.g. mouth, nose, eyes) or non-intact skin have been contaminated with blood or other bodily fluids.
- Mucous membranes/mucosa
The surfaces lining the cavities of the body that are exposed to the environment such as the lining of the mouth and nose.
- Multi-bed room
A room that contains more than one bed.
The acceptable maximum number of beds in a multi-bed room is four. Multi-bed rooms require two clinical wash-hand basins and must have en-suite sanitary facilities. Ideally, an assisted shower room (with WC, shower and general wash-hand basin) and a separate semi-ambulant WC (with general wash-hand basin) both en-suite.
- Negative pressure isolation room
A room which maintains permanent negative pressure. Air flow is from the outside adjacent space (for example corridor) into the room and then exhausted to the outside.
The room should be used to accommodate a patient known or suspected to be infected with a microorganism spread by the airborne route whilst the patient is considered infectious.
- Non-intact skin
Skin that is broken for example by cuts, abrasions, dermatitis, chapped skin, eczema.
- Non-intact skin exposure
An incident in which non-intact skin is exposed to blood or body fluids.
- Non-sterile procedure
Care procedure that does not need to be undertaken in conditions that are free from bacteria or other microorganisms.
- Nosocomial
An infection occurring in a patient during the process of care in a hospital or other health care facility, which was not present or incubating at the time of admission.
- Novel
Scientifically, novel is used to refer to things of recent origin or introduction, such as a novel pathogen.
- Occupational exposure
An occupational exposure is a percutaneous or mucocutaneous exposure to blood or other body fluids.
- Organism
Any living thing that can grow and reproduce, such as a plant, animal, fungus or bacterium.
- Outbreak
- Outpatient
An outpatient is a patient who attends a consultant or other medical/healthcare clinic or has an arranged meeting with a consultant or a senior member of their team out with a clinic session. Outpatient attendances involve treatment or assessment that only take a short time to complete. Outpatient attendances are categorised as new or return (follow-up).
- Overcrowding
Within health and care settings, this is the state of being filled past capacity/comfort and therefore being burdened by excessive demands for services.
- Pandemic
A disease outbreak that occurs over a wide geographical area (such as multiple countries and/or continents) and typically affects a significant proportion of the population.
- Pathogen
Any disease-producing infectious agent.
- Patient cohorting
Placing a group of two or more patients (a cohort) with the same infection/strain in the same bay/ward. Cohorts are created based on clinical diagnosis, microbiological confirmation, epidemiology, and mode of transmission.
- PCR test
Highly accurate tests used to diagnose certain infectious diseases.
- Percutaneous injury
An injury caused by a needle or sharp, instrument, bone fragment, human scratch or bite cutting or puncturing the skin.
- Personal Protective Equipment (PPE)
Equipment a person wears to protect themselves from risks to their health or safety, including exposure to infections, for example disposable gloves and disposable aprons.
- Physical Distancing
Keeping a distance from other people, in order to stop transmission of a disease to another person or other people.
- Pre-symptomatic
The time period when someone has the infection but has not yet developed symptoms but does go on to develop symptoms later in the disease.
- Primary Care setting
These provide the first point of contact in the healthcare system which includes general practice, dentistry, community pharmacies.
- Problem Assessment Group (PAG)
A group that is convened by the Infection Prevention and Control Team (IPCT)/Health Protection Team (HPT) to assess a healthcare incident/outbreak/data exceedence and determine if further action is required.
The assessment and outcome may be:
- HIIAT Green - continue to monitor
- HIIAT Amber/Red - IMT required
- Q
No terms
- Recapping/Re-sheathing
To put a needle or other sharp object back into its plastic sheath or cap. Also known as ‘re-sheathing’.
- Respiratory droplets
A small droplet >5 μm in diameter, such as a particle of moisture released from the mouth during coughing, sneezing, or speaking.
- Respiratory Protective Equipment (RPE)
Respirators are devices that cover the nose and mouth and are designed to filter the air breathed in to protect the wearer from inhaling hazardous substances.
They provide respiratory protection from infectious agents transmissible by the airborne (aerosols) route. FPP3 respirators are recommended for use in UK health and care settings when exposure to aerosols is anticipated.
- Safer sharp
A medical sharps device which has been designed to incorporate a feature or mechanism that minimises and/or prevents the risk of accidental injury. Other terms include (but are not limited to) safety devices, safety-engineered devices and safer sharps devices.
- Safer sharps device
Any device designed to reduce the risk of injury from needles. This may include needle-free devices or mechanisms on a needle, such as an automated resheathing device, that cover the needle immediately after use.
- Sanitary fittings
All sinks and furniture in a bathroom, including a toilet, bath, shower.
- Screening
Performing a test or enquiry to identify individuals at risk of a specific disorder or infection to warrant further investigation or direct preventive action.
- Secondary care setting
Provided by health professionals who generally are not the first point of contact for a patient. These settings are usually hospitals but can also be community-based.
- Secretions
Any body fluid that is produced by a cell or gland such as saliva or mucous, for a particular function in the organism or for excretion.
- Segregated
Physically separating or isolating from other people.
- Sepsis
A life-threatening condition that arises when the body’s response to a severe complication of infection for example pneumonia (lung infection) injures its own tissues and organs. This can lead to multiple organ failure and death. Early recognition, treatment and management is key to successful patient outcomes.
- Sharp
A ‘sharp’ is a device or instrument used in healthcare settings with sharp points or edges, such as needles, lancets and scalpels which have the potential to cause injury through cutting or puncturing the skin.
- Sharps incident
-
A type of percutaneous injury caused by a sharp instrument or device which cuts or penetrates the skin.
- Sharps injury
See percutaneous injury.
- Significant occupational exposure
A percutaneous, mucocutaneous or non-intact skin (abrasions, cuts, eczema) exposure to blood or other body fluids from a source that is known (or later found to be) positive for a bloodborne virus infection.
- Significant sharps incident
An incident which involves a used needle that has exposed, or may have exposed, the employee to blood/body fluids.
- Single-bed room
A room with space for one patient and usually contains as a minimum: a bed; locker/wardrobe; clinical wash-hand basin.
Single-bed rooms should also have en-suite sanitary facilities comprising of a shower, WC and a general wash-hand basin.
- Skin integrity
Skin being intact, and in an unimpaired condition.
- Source control
This term encompasses all physical measures used to control the transmission of an infectious agent.
- Spore
A reproductive cell produced by fungi and some types of bacteria under certain environmental conditions. Spores can survive for long periods of time and are very resistant to heat, drying and chemicals.
- Staff cohorting
A dedicated team of healthcare staff who care for a cohort of patients, and do not care for any other patients.
- Standard infection control precautions (SICPs)
These are a group of basic infection prevention and control practices that need to be adopted by all staff in health and care settings, irrespective of infectious status of patient.
- Sterile
Free from live bacteria or other microorganisms.
- Sterile procedure
Care procedure that is undertaken in conditions that are free from bacteria or other microorganisms.
- Sterilisation
The procedure of making some object free of all germs, live bacteria or other microorganisms (usually by heat or chemical means).
- Surgical face mask
A disposable fluid-resistant mask worn over the nose and mouth to protect the mucous membranes of the wearer’s nose and mouth from splashes and infectious droplets and to protect patients. When recommended for infection control purposes a 'surgical face mask' typically denotes a fluid-resistant (Type IIR) surgical mask.
- Surgical hand antisepsis
Surgical scrubbing or surgical rubbing. More thorough than routine hand hygiene. In addition to the removal of visible soiling and transient bacteria, it prevents the growth of resident microbial skin flora before performing an invasive procedure.
- Surgical rubbing
The process of surgical hand antisepsis using ABHR prior to performing a sterile or surgical procedure. An alternative to surgical scrubbing when hands are not visibly soiled.
- Surgical scrubbing
The process of removing debris and sterilising hands prior to performing a sterile or surgical procedure.
- Surgical site infection
This is an infection which occurs after the surgery at the site of the surgical incision due to introduction and multiplication of pathogens at the surgical site.
- Swan-neck
Way of closing bag by twisting the top of the bag (must not be more than 2/3 full), looping the neck back on itself, holding the twist firmly, and placing a seal over the neck of the bag (such as with a tag).
- Terminal decontamination
Cleaning/decontamination of the environment following transfer/discharge of a patient, or when they are no longer considered infectious, to ensure the environment is safe for the next patient or for the same patient on return.
- Touch surfaces
These are surfaces that are frequently touched by different people throughout the day and are therefore more likely to be contaminated with bacteria or viruses for example doorknobs, tables, phones, which can then easily transfer to the user.
- Transmission-based precautions (TBPs)
These are additional measures that are used in conjunction with SICPs when caring for patients with a known or suspected infection or colonisation.
- U
No terms
- Vaccination
Treatment with a vaccine to produce immunity against a disease.
- Vaccine
A suspension that is administered in order to stimulate the immune response of the body against an infectious agent.
- Vascular access devices
Any medical instrument used to access a patient’s veins or arteries such as a Central Venous Catheter or Peripheral Vascular Catheter.
- Ventilation
Ventilation is a means of removing and replacing the air in a space. In its simplest form this may be achieved by opening windows and doors.
- Viral load
The viral load or viral burden is a numerical expression of the amount of virus present in biological fluids or environmental specimens.
- Ward
An area forming a division of a care setting (or a suite of rooms) shared by patients who need a similar type of care.
- X
No terms
- Y
No terms
- Z
No terms